What you need to know
Slit Lamp Viewing:
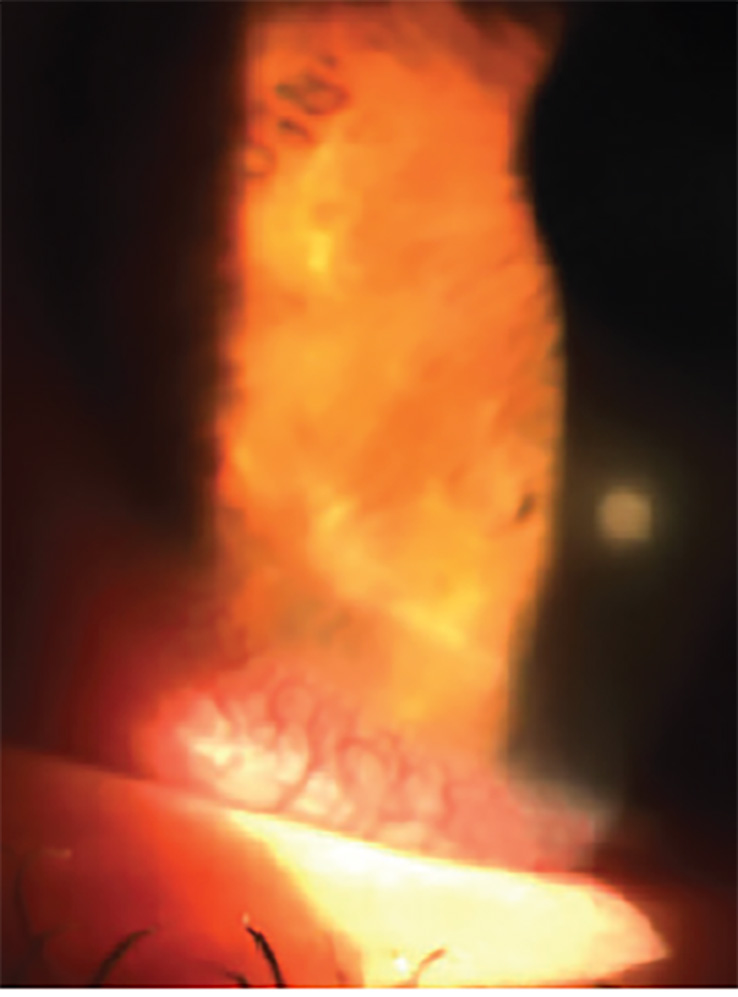
• Direct focal illumination • Medium/high magnification (16 – 25x) in white light and then fluorescein with blue cobalt filter and yellow barrier filter • White light optic section to assess depth
Describing clinical appearance:
- Location: Superior, inferior, nasal, temporal; central or peripheral
- Size: Measure/estimate diameter and depth and/or capture image
Incidence:
- Daily wear (DW) 1 – 5% (SiHys > hydrogels)
- Overnight wear 1 – 13% (hydrogel), 3.3 – 5.4% (SiHys)
Aetiology:
- Inflammatory reaction with focal excavation of the epithelium, and infiltration and necrosis of the anterior stroma (Bowman’s layer intact).
- Inflammatory response to exotoxins from gram positive bacteria (esp. staphylococcus spp).
- Due to: bacterial contamination, closed eye, tight lens, poor hygiene, lid margin disease.
- Risk factors: high ametropia (>5D), younger age (15-25 years), case contamination, environmental influences.
Symptoms:
- Up to 50% asymptomatic and unaware of complication
- Lens intolerance, foreign body sensation, photophobia, lacrimation, episodes of acute red eye
- Symptoms reduce after lens removal
Signs:
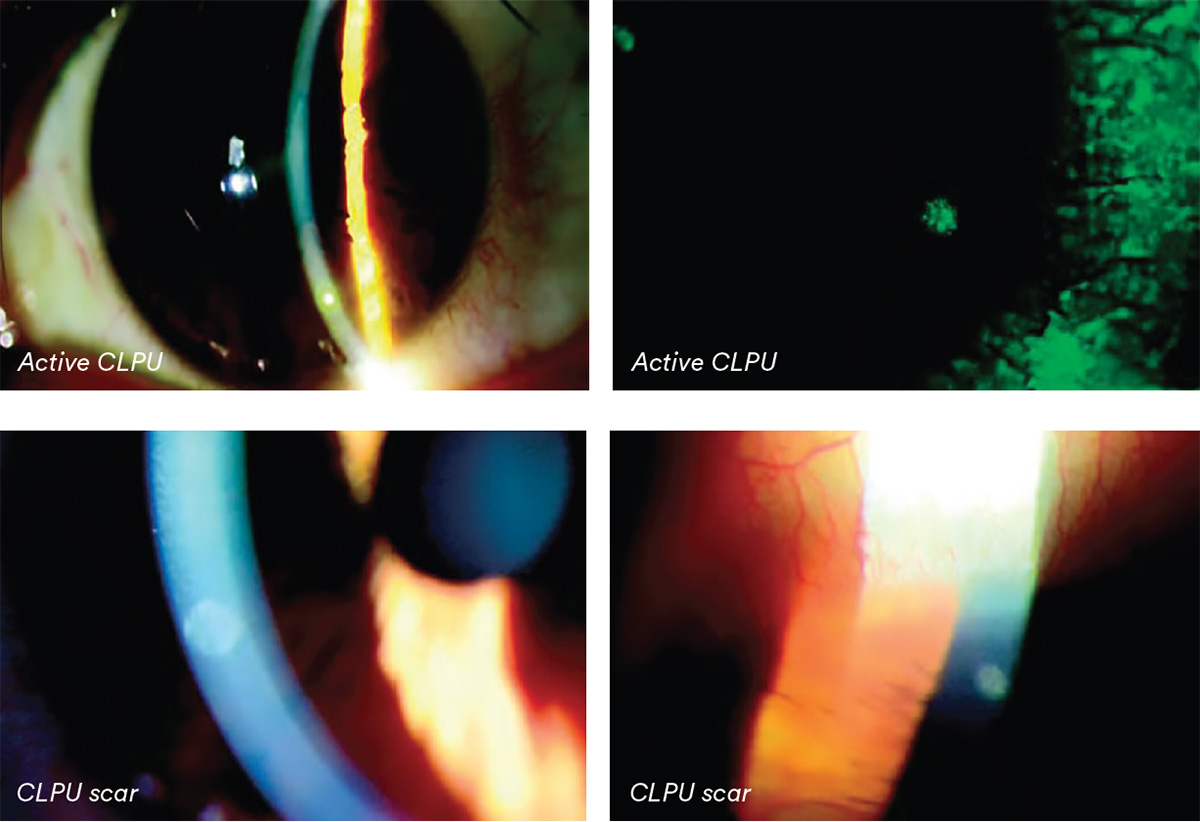
- Moderate, localised hyperemia
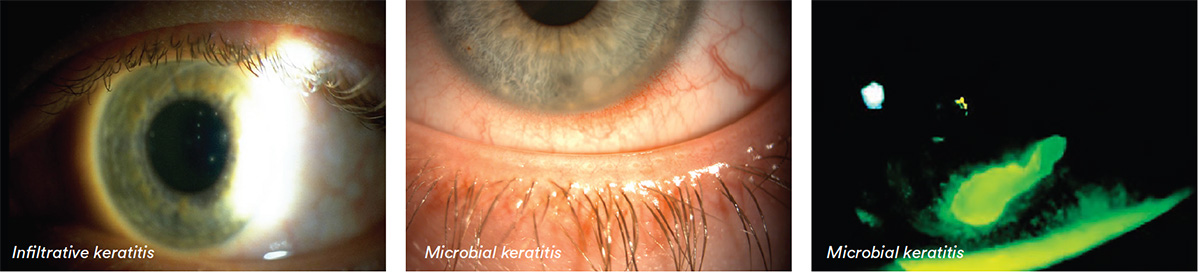
- Sterile infiltrate — peripheral / mid- peripheral, small (0.2 — 2.0mm), single focal, circular, stains and diffuse infiltration (in acute phase), can be multiple, although rare
- Anterior chamber reaction if severe (rare)
What you need to recommend to your patients
Management:
- Self-limiting on removal but close monitoring for 24 hours to ensure differential diagnosis from infected MK. If central, >1mm and pain, treat suspiciously
- Follow up depends on severity
- Cease lens wear until epithelium intact over lesion (up to 14 days)
- Ocular lubricants to prevent lid rubbing over affected area and dilute bacterial toxins
- Oral analgesics to reduce discomfort (if severe)
- Severe cases, acute red eye or no resolution with lens removal — consider prophylactic antibiotic with/without anti-inflammatory (esp. if infiltrates on visual axis)
- Eliminate bacterial source — lid hygiene, and review hygiene practices
- Increase lens replacement frequency, change care system, refit into DD, or rigid corneal lens
- If in planned overnight wear, consider limiting to six nights at a time or DW
- Review case hygiene and replacement
Prognosis:
- Good if visual axis not involved — single, spherical scar often remains, but can fade with time
- Certain subjects prone to recurrent inflammation (10 - 25%)
Differential Diagnosis:
Infiltrative keratitis (IK), microbial keratitis (MK), corneal dystrophies, herpes simplex keratitis (HSK), stromal scar
Further reading
- Aasuri M et al. Differential diagnosis of microbial keratitis and contact lens-induced peripheral ulcer. Eye Contact Lens 2003 Jan; 29(1 Suppl): S60-62; discussion S83-84, S192-194
- Chalmers RL et al. Risk factors for contact lens complications in US clinical practices. Optom Vis Sci 2010; 87(10): 725-735
- Dumbleton K et al. Severity and management of contact lens related complications with continuous wear of high-Dk silicone hydrogel lenses. Optom Vis Sci 2000; 77(12s): 216
- Dumbleton K. Adverse events with silicone hydrogel continuous wear. Cont Lens Ant Eye 2002; Sep 25(3): 137-46 • Efron N, Morgan P. Can subtypes of contact lens-associated corneal infiltrative events be clinically differentiated? Cornea 2006 Jun; 25(5): 540-544
- Grant T et al. Contact lens induced peripheral ulcers during hydrogel contact lens wear. CLAO J 1998; 24: 145-51
- Holden B et al, Contact lens-induced peripheral ulcers with extended wear of disposable hydrogel lenses: histopathologic observations on the nature and type of corneal infiltrate. Cornea 1999; 18: 538-43
- Ozkan J et al. Risk factors for corneal inflammatory and mechanical events with extended wear silicone hydrogel contact lenses. Optom Vis Sci 2010; 87(11): 847-853
- Radford C et al. Risk factors for non-ulcerative contact lens complications in an ophthalmic accident and emergency department: a casecontrol study. Ophthalmology 2009; 116(3): 385-992
- Wu P et al. The causes of and cures for contact lens-induced peripheral ulcer. Eye Contact Lens 2003; 29: S63-6; discussion S83-4, S192-4
- Click here to review our Slit Lamp Techniques Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answers at the foot of the page to see whether it’s correct. Good luck!
History:
Patient DR is a 38-year-old car mechanic who has worn hydrogel daily wear lenses, seven days a week for 10 years.
He attends for a check-up for the first time in two years and initially reports no complaints about his lenses. On closer questioning he reveals that his right eye has been sore and red in the past few days. His fingers are stained with nicotine and his hands show signs of poor hygiene, with dirty fingernails. He is uncertain of the name of care solution he uses and no lens case has been brought to the appointment.
Questions:
1. How would you describe this patient’s CLPU?
A. Inferior, central, approx. 1.5mm
B. Inferior, mid peripheral, approx. 0.5mm
C. Superior, peripheral, approx. 0.5mm
D. Nasal, central, approx. 2.0mm
2. What sign or symptom of CLPU is especially pertinent to its differential diagnosis?
A. Hyperaemia
B. Mid peripheral/peripheral location
C. Discomfort
D. Lacrimation
3. Which of the following signs and symptoms might determine whether you refer a patient with CLPU?
A. Central location
B. >1mm in diameter
C. Pain
D. All of these
4. Which of the following management options would you be most likely to choose first for this patient?
A. Discontinue lens wear and monitor closely for 24 hours before deciding on management
B. Discontinue lens wear for two weeks before seeing again then decide on managements
D. Refit with DD lenses and advise on hand hygiene
C. Refer urgently for ophthalmological investig
Answers:
1. Correct answer is B. Grade 2
2. Correct answer is B. CLPU is characterised by sterile infiltrates in a mid peripheral/ peripheral location
3. Correct answer is D. All of these signs and symptoms should be treated suspiciously to ensure differential diagnosis from MK
4. Correct answer is A. CLPU is often self-limiting on lens removal but close monitoring for 24 hours is needed to exclude MK