What you need to know
Slit Lamp Viewing:
• Diffuse beam • Medium magnification (16x) • Direct illumination • Fluorescein to assess
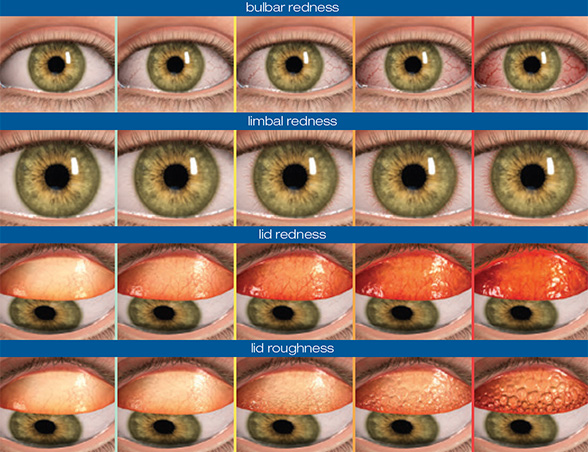
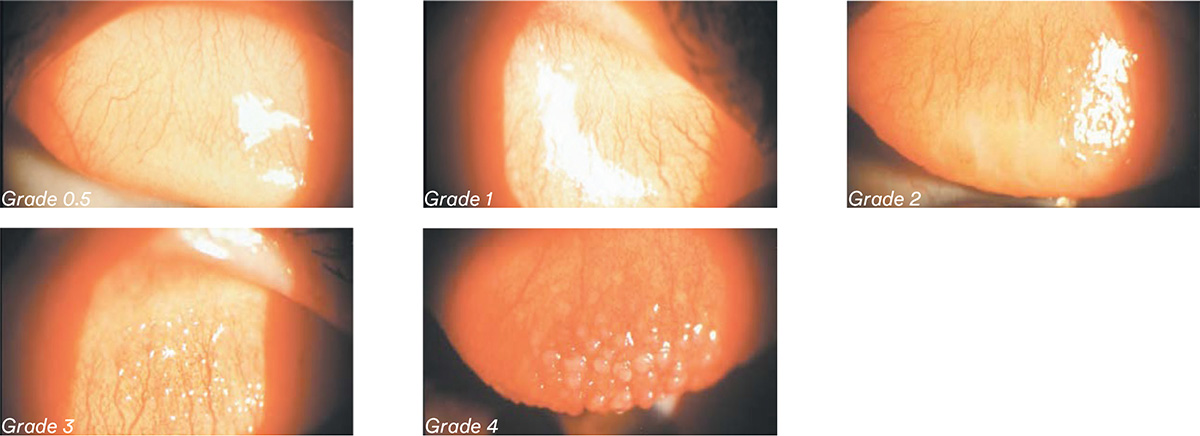
Grading:
Grade 0: Few vessels on surface; smooth, even conjunctiva
Grade 1: Small papillae, few vessels on surface, uneven slit lamp surface reflection
Grade 2: Loss of transparency, small papillae, uneven slit lamp surface reflection
Grade 3: Papillae with vessels visible
Grade 4: Papillae with staining and vessels
Incidence:
- Variable time of onset and severity; varies over years with different lenses and care regimens.
- 2% rigid corneal lenses, 2 – 15% hydrogel daily wear, 2 – 19% hydrogel overnight wear, 2 – 7% SiHys (silicone hydrogels).
- Significantly reduced since the introduction of frequent replacement CLs.
- Increased incidence with overnight wear, non-planned replacement and higher modulus materials (mechanical related).
Aetiology:
- Conjunctival inflammatory condition associated with CLs or trauma.
- Immunological response — delayed hypersensitivity (denatured deposits, solution sensitivity).
- Mechanical response (lens design or material modulus, prostheses and sutures).
- Associated with atopy and MGD.
Symptoms:
- Lens awareness, CL intolerance, foreign body sensation, itching which may increase on lens removal
- Mucus formation, visual disturbance (lens dislocation, deposition and mucus)
Signs:
- Papillae (>0.3mm) on upper tarsal conjunctiva with central vascular tuft,mucus discharge, tarsal conjunctival hyperaemia and oedema
- Displaced CL and excessive movement with poor surface wetting and deposits
- Location of papillae tends to be confined to lesser area tarsal conjunctiva with SiHys (localised)
What you need to recommend to your patients
Management:
- Manage if ≥ grade 2 or ≥ 1 grading interval increase or if symptoms
- Lens wear can continue if symptoms allow
- Improve lens hygiene (ensure rub and rinse step with MPS (multipurpose solution), change care system to preservative free)
- Increase lens replacement frequency (ideally daily disposable), replace existing lenses
- Alter lens design or material (reduce edge clearance and thickness of rigid corneal lenses, fit lower modulus soft lens material)
- Introduce lid hygiene if signs of lid margin disease
- If severe, temporary cessation of lens wear with topical mast cell stabilisers or steroids in cases where lens wear is essential (eg keratoconus)
Prognosis:
- Good, especially with frequent replacement lenses, although papillae can remain for months or years.
- Better with early detection — resolves within 2 – 3 weeks if mechanical, longer if inflammatory cause.
- Up to 60% recurrence with SiHy EW (extended wear).
Differential Diagnosis:
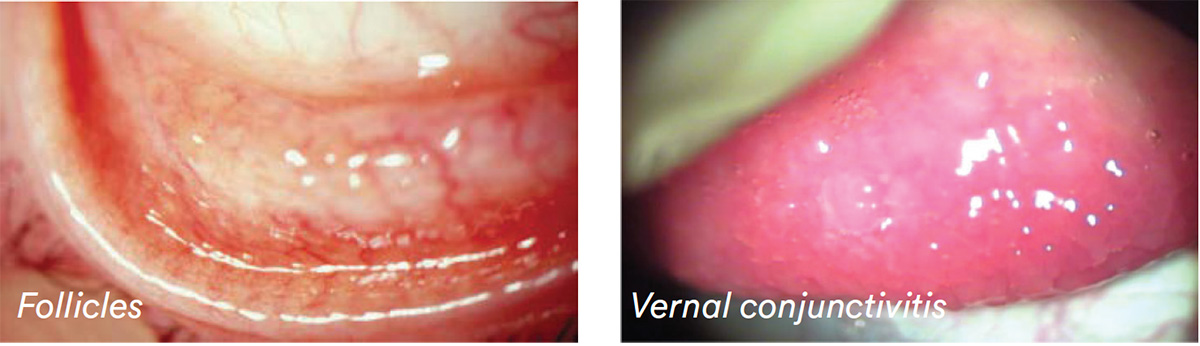
- Follicles — vessels on the outside of the enlarged area of tissue.
- Inferior tarsal conjunctivitis — not CL related.
- Seasonal allergic conjunctivitis.
- Vernal conjunctivitis — no vessels (young males, both inferior and upper tarsus).
- Giant papillary conjunctivitis caused by other reasons, for example mechanical irritation from protruding corneal sutures.
Further reading
- Dumbleton K. Adverse events with silicone hydrogel continuous wear. Cont Lens Ant Eye 2002; Sep 25(3): 137-46
- Dumbleton K. Noninflammatory silicone hydrogel contact lens complications. Eye & contact lens 2003; 29(1 Suppl): S186–S194
- Efron N. Contact lens induced papillary conjunctivitis. Optician 1997; 213(5583): 20-27
- Jurkus J. Contact lens induced papillary conjunctivitis. In Anterior Segment Complications of contact lens wear 1994; Vol 1 (ed, Silbert J) pp 163—177. Churchill Livingstone Inc, New York
- Lin M, Yeh T. Mechanical complications induced by silicone hydrogel contact lenses. Eye & CL 2013; 39(1): 115–124
- Skotnitsky C et al. General and local contact lens induced papillary conjunctivitis (CLPC). Clin Exp Optom 2002; 85: 193-7.
- Skotnitsky C et al. Two presentations of contact lens-induced papillary conjunctivitis (CLPC) in hydrogel lens wear: local and general. Optom Vis Sci 2006; 83: 27-36.
- Sorbara L et al. Contact lens induced papillary conjunctivitis with silicone hydrogel lenses. Cont Lens Anterior Eye 2009; 32: 93-6.
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answers at the foot of the page to see whether it’s correct. Good luck!
History:
Patient CB is a 29-year-old management trainee who has worn the same brand of monthly replacement silicone hydrogel lenses since she started wearing contact lenses 8 years ago. She visits your practice for the first time complaining of severe itching with and without her lenses, ‘sticky’ eyes and having to remove the lenses after 6 hours’ wear.
Questions:
1. What slit lamp technique would you use to examine this patient’s upper lids?
A. Narrow beam
B. White light and fluorescein
C. High magnification
D. White light only
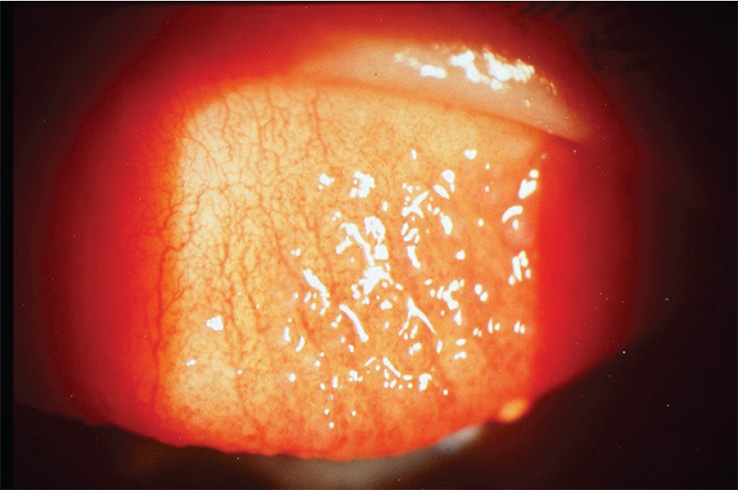
2. What grade would you give to her lid roughness?
A. Grade 2.5
B. Grade 3.0
C. Grade 3.5
D. Grade 4.0
3. What material properties are associated with lid roughness?
A. Lens modulus
B. Surface characteristics
C. Lens design
D. All of these
4. Which of the following management options would you be most likely to choose?
A. Switch to daily disposable lenses
B. Refit with RGP lenses
C. Discontinue lens wear permanently
D. Continue with these lenses, reduce wearing time
Answers:
1. The correct answer is B. Evert the lids and use both white light and fluorescein (right), with a diffuse beam and medium magnification.
2. The correct answer is C. The patient’s lid shows papillae with vessels, and should be recorded grade 3.5 lid roughness.
3. The correct answer is D. These material properties are all implicated as contact lens related causative factors in lid roughness
4. The correct answer is A. Daily disposables may be the best option in this particular case, especially during the hayfever season