What you need to know
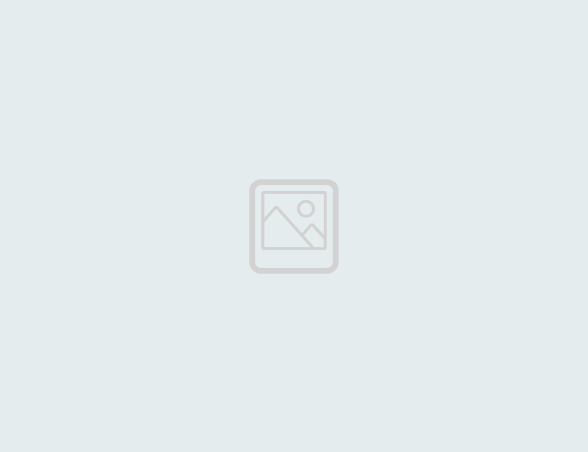
Slit Lamp Viewing:
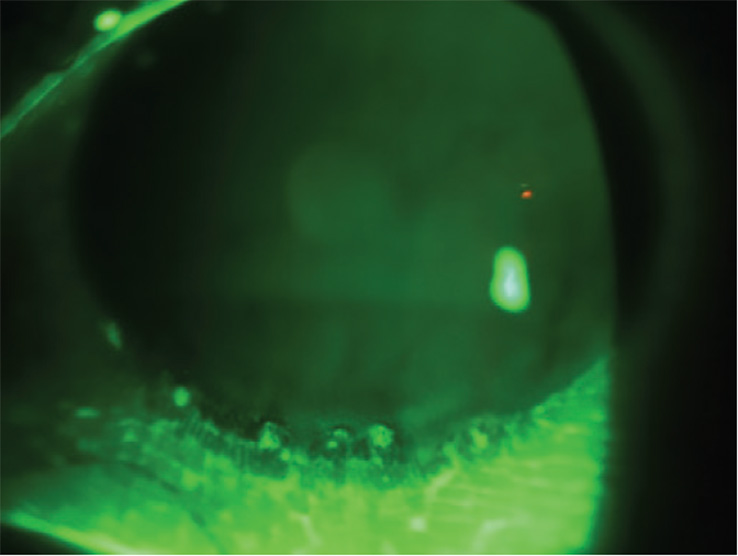
• Direct focal illumination • Medium/high magnification (16 – 25x) in white light and then with fluorescein with blue cobalt filter and yellow barrier filter • White light optic section to assess depth
Describing clinical appearance:
- Location: Superior, inferior, nasal, temporal; central or peripheral
- Size: Measure/estimate size and depth and/or take a digital image
Incidence:
- 3% DW soft lens wear, 2.5-6% EW soft lens wear, 2x increased risk with reusable SiHys (DW or overnight wear), <0.5% DD wear
- Can occur in non-lens wearers
Aetiology:
- Infiltrative event other than those identified as Contact lens peripheral ulcer (CLPU), Contact lens associated red eye (CLARE) or Microbial keratitis (MK)
- Sterile corneal infiltrates — inflammatory reaction with anterior stromal infiltration due to: hypoxia, closed eye, tight lens, bacterial toxins, denatured lens deposits, solution sensitivity, lid margin disease, poor hygiene, allergic reaction, adenoviral infection, mechanical trauma
Risk factors:
High ametropia (>5D), younger age (15-25 years), older age (>50 years), males, lens case contamination, environmental influences, previous CIE, use of MPS, bacterial bioburden, solution induced corneal staining (SICS), smoking (current or past)
Symptoms:
- Lens intolerance and foreign body sensation
- Photophobia and lacrimation
- Episodes of acute red eye
Signs:
- Moderate bulbar redness, focal stromal infiltrates (described as marginal keratitis if at 4 and 8 o’clock and due to staphylococcal exotoxins from lid margins)
- With or without epithelial involvement (staining) and can be bilateral
What you need to recommend to your patients
Management:
- Temporary discontinuation of lens wear until infiltrates disappear and no other signs or symptoms
- Careful monitoring, ocular lubricants, lid hygiene
- No medication required (in most cases) topical antibiotic and anti-inflammatory may be considered if severe and/or on visual axis
- Resolution often within 14 days (longer with greater severity)
- Reduce lid margin bioburden and organism contamination
- Address case hygiene and replacement
- For s olution induced contact lens staining (SICS), alter combination of SiHy and Multipurpose solution (MPS), switch to Hydrogen Peroxide system, or change to DD
- Once resolved, change to DW, increase lens oxygen performance, loosen lens fit, increase lens replacement frequency, change care system, review lens handling and hygiene
Prognosis:
- Rarely scars so prognosis good as long as visual axis not involved — resolves within 2 weeks.
- Small residual scars may result depending on cause and depth of infiltration.
- Certain subjects prone to recurrent inflammation — stop any overnight wear.
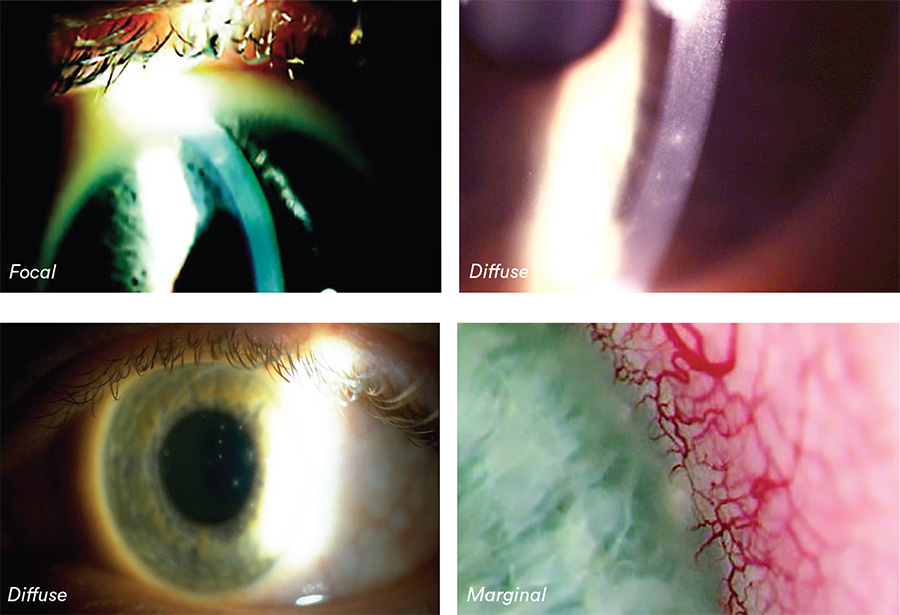
Differential Diagnosis:
Microbial keratitis (MK), epidemic keratoconjunctivitis, corneal dystrophies, corneal nerves, herpes simplex, old corneal scar.
Further reading
- Carnt N et al. Solution toxicity in soft contact lens daily wear is associated with corneal inflammation. Optom Vis Sci 2007; 84(4): 309-315
- Chalmers R et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci 2011; 52(9): 6690-6696
- Chalmers R et al. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci 2012; 89 (3): 316-325
- Chalmers R et al. Rates of adverse events with hydrogel and silicone hydrogel daily disposable lenses in a large postmarket surveillance registry: The TEMPO registry. Invest Ophthalmol Vis Sci 2015; 52(1): 654-653
- Ozkan J et al. Risk factors for corneal inflammatory and mechanical events with extended wear silicone hydrogel contact lenses. Optom Vis Sci 2010; 87 (11): 847-853
- Papas EB et al. Complications associated with care product use during silicone daily wear of hydrogel contact lens. Eye Contact Lens 2007; Nov 33(6 Pt 2): 392-393; discussion 399-400
- Radford C et al. Risk factors for nonulcerative contact lens complications in an ophthalmic accident and emergency department: a case control study. Ophthalmology 2009; 16: 385-392
- Steele KR, Szczotka-Flynn L. Epidemiology of contact lens-induced infiltrates: an updated review. Clin Exp Optom 2017; 100: 473-481
- Sweeney D et al. Clinical characterization of corneal infiltrative events observed with soft contact lens wear. Cornea 2003; 22: 435-42.
- Szczotka-Flynn L, Diaz M. Risk of corneal inflammatory
- Click here to review our Slit Lamp Techniques Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answers at the foot of the page to see whether it’s correct. Good luck!
History:
Patient TP a 23-year-old trainee accountant, is a -7.00D myope who has been wearing monthly replacement SiHy lenses for up to 30 nights’ extended wear over the past nine months.
She attends for an unscheduled appointment complaining of repeated episodes of sore, red, watery eyes over the previous few weeks and is now unable to tolerate her lenses for more than four hours a day.
Questions:
1. What slit-lamp techniques might you use to examine this patient’s cornea?
A. Direct illumination
B. Low magnification
C. Indirect illumination
D. Diffuse beam
2. What is the incidence of Infiltrative Keratisis for this modality of contact lens wear?
A. <0.5%
B. 2.5 - 6%
C. 3%
D. >6%
3. What risk factor may be associated with infiltrative keratitis in this patient?
A. High myopia
B. Overnight wear
C. Age
D. All of these
4. Which of the following management options would you be most likely to choose?
A. Continue lens use but on a daily wear basis
B. Discontinue lens wear for two weeks before seeing again. Then, if resolved, refit with 2-weekly daily wear SiHys
C. Refer urgently for ophthalmological investigation
D. Discontinue lens wear and prescribe antibiotic drops
Answers:
1. Correct answer is A. Direct focal illumination with medium/high magnification is the best technique for assessing Infiltrative keratitis
2. Correct answer is B. The incidence of Infiltrative Keratitis in extended wear is reported as 2.5-6%
3. Correct answer is D. All of these are potential risk factors in this patient although the aetiology may be multi-factorial
4. Correct answer is B. In mild cases, infiltrates will often resolve without treatment when lens wear is discontinued. Once resolved, daily wear and more frequent replacement are the most appropriate options, along with improved hygiene