By Christine Purslow and Simon Donne
Why initiate a contact lens conversation
As eye care practitioners we have a duty of care to offer patients the opportunity to update their vision correction if we feel they would benefit. We should ensure all our contact lens wearers are as comfortable as possible, with minimal impact on ocular physiology, no matter what their visual correction or history of wear.
It is our role to encourage patients to voice their concerns and explain there is a range of options available to maintain healthy and comfortable contact lens wear
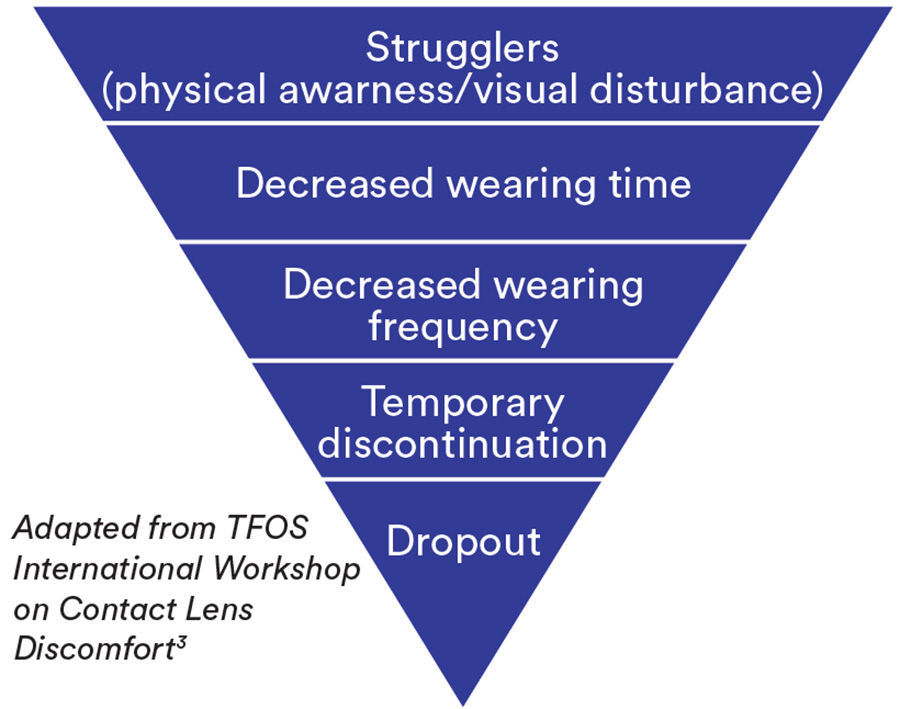
Managing the dropout
Discomfort during lens wear is the main reason for dropping out of contact lenses.1,2
Many contact lens wearers start and stop lens wear repeatedly over several years.1
A seemingly satisfied patient can be just a few steps away from giving up on contact lenses due to discomfort
Patient and eye care practitioner relationship: a maze of assumptions and unspoken thoughts
Practitioner
- May assume that if no dissatisfaction is expressed then everything is ‘fine’
- May assume patients will mention any significant milestones, events or activities occurring in their life
Patients
- May assume if we don’t ask it can’t be important
- May feel silly or anxious mentioning lens discomfort – they may think all lenses are the same and are supposed to feel like that. They may also come to have accepted this as ‘normal’.
- May say all is ‘fine’ especially as they may feel expressing dissatisfaction could lead to no longer being able to wear lenses
- May assume that we would advise them of developments/offer upgrades if needed
- May assume that ‘no change needed’ means current updates aren’t relevant to them
What to look and listen for
Checking compliance though observation

Asking questions to gain an honest answer is the challenge.‘Do you wash your hands before handling your lenses?’ often produces a reflex ‘yes’ answer. Try observing first:
- Observe patients when removing their lenses
- Observe their care regime – this can reveal non compliance regarding solutions and use of tap water, or hand and case hygiene.
Observation provides an ideal opportunity to reinforce the need for hand hygiene and good lens care. It can allow you to ask more questions such as whether a patient may prefer to change to daily disposables for convenience.
Look out for clinical situations
- There may be situations when an alternative option could supplement existing wearing modalities
- Allergy sufferers experiencing symptoms in hay fever season – think about suggesting daily disposables5
- Patients occasionally sleeping in lenses – discuss increased risks of overnight wear6,7
- Patients who are travelling a lot or going on holidays where solutions are an inconvenience may benefit from the convenience of a daily disposable at this time
Look for non-verbal clues to dissatisfaction

- Watch for ‘strugglers’ – making unscheduled appointments, collecting lenses or arriving for aftercare appointments wearing spectacles
- Make note of any reduction in purchasing patterns, or delayed collection of their contact lens supply.
- Look for patients who seem unhappy or reluctant whilst waiting to see you
What to say and do
Avoid closed questions initially

Whilst closed questions can be useful, open questions typically ellicit more information intially.
A simple ‘how are your lenses?’ may result in ‘good’ or ‘fine’ as patients may fear being told they have to pay more for lenses, reduce their wearing time or worse still, stop wearing lenses.
Asking the time they tend to put lenses in and take them out rather than ‘how many hours do you wear your lenses for?’ can present a more realistic picture.
Closed questions have a place when trying to gain specific information from a patient.
Keep yourself and your team up-to-date

- Holding regular staff training sessions and fitting them with the latest contact lenses will inspire confidence when talking to patients.
- Reassure patients that their current lenses are fine but you can offer them something better. Use your lens knowledge to describe both the features and benefits of the new lenses available.
- Contact lenses technology changes and evolves and it is often useful to ask yourself: ‘If I were fitting this patient for the first time today - which lens would I recommend?’ In some cases you can then reassure the patient that they are still in the lens you feel is right for them, but in other cases, you may be able to offer a better option.
Using a grading scale
Ask patients to grade their comfort on a scale of 0-10 on application and at the end of day. This can help to overcome reluctance to report symptoms.
Early changes or reductions in comfort scores over subsequent visits can be useful markers in preempting concerns.
Elicit concerns using open questions and empathy
‘You take your lenses out at six every evening – is that because you want to or because you have to?’
‘You mentioned you almost feel guilty wearing your lenses for so long during the day – modern lenses allow virtually as much oxygen to your eye as if you weren’t wearing any lenses at all’
Highlight signs to patients
Sometimes there can be a disparity between signs and symptoms. For example, patients can often display limbal redness in the absence of symptoms. Try asking ‘do you feel that your eyes ever look red when you look in the mirror? – if they say yes you can follow with ‘would you like me to try and improve that for you?’