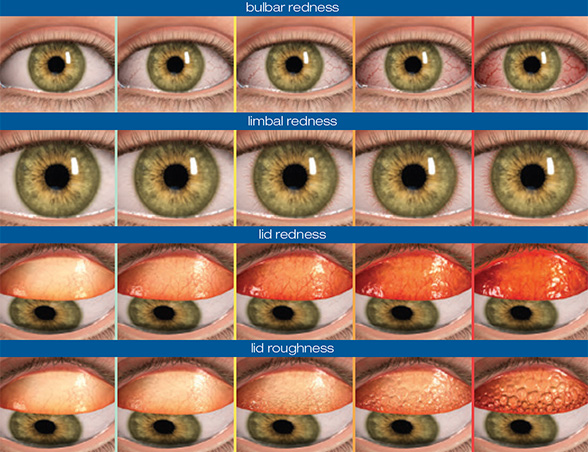
What you need to know
Slit Lamp Viewing:
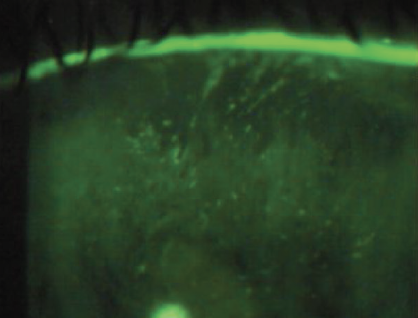
• Direct illumination, parallelepiped or diffuse • Medium/high magnification (16 – 30x) • Fluorescein with blue cobalt filter and yellow barrier filter.
Grading position:
Superior, nasal, inferior, temporal, central
Grading extent:
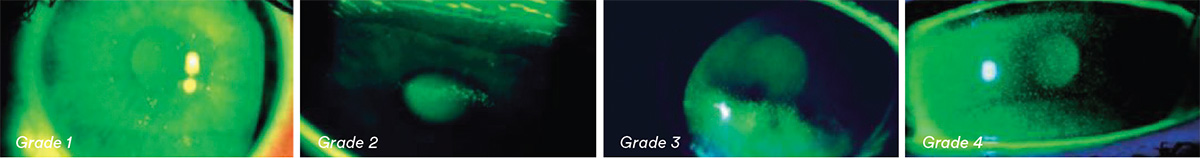
Grade 0: None
Grade 1: 1 – 20 punctate diffuse spots
Grade 2: 21 – 40 punctate diffuse spots
Grade 3: > 40 diffuse spots and/or coalescing patches
Grade 4: Dense confluent patches
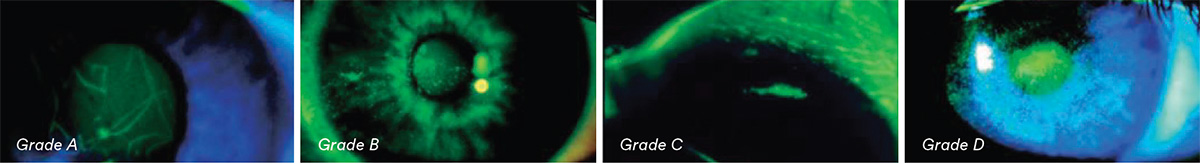
Grading extent:
Grade A: No stromal diffusion
Grade B: Stromal diffusion delayed (30 – 60 seconds)
Grade C: Stromal diffusion immediate but moderate
Grade D: Stromal diffusion immediate and widespread
Incidence:
- Common in all CL wearers (up to 60%) but often clinically insignificant
- More common in Ortho-K as the lens design is intended to produce compressive forces on the cornea
- Some degree also seen in non-CL wearers (35%)
Aetiology:
- Mechanical — trauma, foreign body, damaged lens, lens edge, material stiffness, thick lens design, Ortho-K lens wear, scleral lens wear
- Exposure — disruption of tear film and subsequent desiccation
- Metabolic — hypoxia, hypercapnia (tissue acidosis and desquamation of epithelial cells)
- Solution induced corneal staining (SICS) seen 2-4 hours after insertion with some SiHy and multi-purpose solution (MPS) combinations
- Toxic — care regimen hypersensitivity (1-10% hydrogel lens wearers)
- Allergic — delayed or immediate hypersensitivity reaction
- Infectious systemic disease, poor general health (e.g. influenza, throat infection)
Symptoms:
- Can be asymptomatic – depends on etiology and severity; for most cases of grade 3 or 4 there would be some discomfort or even pain
- Symptoms may include CL intolerance, reduced wearing time, dryness, itching
- Reduced vision if significant and located over visual axis
- Lacrimation
Signs:
- Superficial punctate epithelial erosions (extent, depth and location depends on etiology)
- Bulbar conjunctival hyperemia
- Tarsal conjunctival changes
- Lacrimation
- Ortho-K:
- apparent at lens removal and throughout the day
- central staining more likely when correcting myopia; paracentral staining more likely when correcting hyperopia
- exacerbated in new Ortho-K wearers
What you need to recommend to your patients
Management:
- Manage if ≥ Grade 2 or if ≥ 1 grading scale increase
- Remove lenses until resolved
- Consider medical intervention/treatment for Grades 3 and 4 if related to trauma/mechanical causes or infection/inflammation
- Ocular lubricants to reduce symptoms
- Isolate cause and manage — change care system, refit/replace lens, improve oxygen performance, blinking, rewetting drops
- For SICS: ensure a rub & rinse step, alter combination of SiHy and MPS, switch to non- preserved solution or change to DD lens

- Ortho-K:
- Advise instilling aqueous ocular lubricant and gently nudging the lens with the eyelids to mobilise lens before removing
- If new presentation in an existing Ortho-K wearer consider possible lens spoilage/damage/warpage – protein clean lens and if not resolved consider lens replacement
- Grade 1 or 2: Acceptable if confident that staining is lens induced (mechanical) – reinforce advice on lens removal
- Grade 3: Assess in the afternoon to verify staining resolves during the day.
- Grade 4: Discontinue wear until resolved and consider prophylactic antibiotic if there is evidence of epithelial break
- If mechanical-related staining is persistent consider altering lens parameters to reduce mechanical pressure
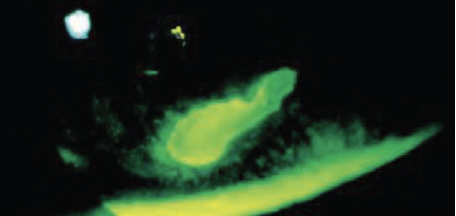
- Scleral lenses:
- Assess whether the lens is bearing on the cornea
- Central lens bearing or lens fenestrations causing abrasion – increase lens sagittal height
- Para-central lens bearing – increase corneal, peripheral and limbal clearance alongside steepening the transition zone
- Hypoxia – increase lens material oxygen transmissibility
- Toxic reaction to solutions – consider change to non-preserved solutions
- Post lens fluid reservoir containing debris – verify compliance
Prognosis:
Good (unless Bowman’s membrane penetrated and subsequent residual scarring)
Differential Diagnosis:
- Infectious keratitis (left),
- Dry eye or ocular surface disease, infectious keratitis (left), mechanical insult (eg: from fingers when applying or removing lens, or from excessive eye rubbing)
Further reading
- Andrasko G, Ryen K. Corneal staining and comfort observed with traditional and silicone hydrogel lenses and multipurpose solution combinations.
- Optometry 2008 Aug; 79(8): 444-454
- Bron AJ et al. Clinical staining of the ocular surface: mechanisms and interpretations. Prog Retin Eye Res 2015; Jan 44: 36-61
- Carnt N et al. Solution toxicity in soft contact lens daily wear is associated with corneal inflammation.
- Optom Vis Sci 2007; Apr 84(4): 309-315
- Efron N. Putting vital stains in context. Clin Exp Optom 2013; 96:400-21.
- Fadel D. Scleral lens issues and complications related to a nonoptimal fitting relationship between the lens and ocular surface. Eye Contact Lens 2019; 45: 152-163
- Fonn D et al. Corneal staining as a response to contact lens wear. Eye Contact Lens 2010; Sep 36(5): 318-321
- Jones L et al. Asymptomatic corneal staining associated with the use of balafilcon silicone-hydrogel contact lenses disinfected with a polyaminopropyl biguanide-preserved care regimen.
- Optom Vis Sci 2002; Dec 79(12): 753-61
- Keir N et al. Clinical performance of different care systems with silicone hydrogel contact lenses
- Cont Lens Ant Eye 2010; Aug 33(4): 189-195
- Morgan P, Maldonado-Codina C. Corneal staining: do we really understand what we are seeing? Cont Lens Anterior Eye 2009; 32: 48-54.
- Peterson R et al. Impact of a rub and rinse on solution-induced corneal staining. Optom Vis Sci 2010; Dec 87(12): 1030-1036
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answer at the foot of the page to see whether it’s correct. Good luck!
History:
Patient GC is a 38-year-old retail assistant who has worn silicone hydrogel lenses successfully for 3 years and has been symptom-free at each aftercare visit. He comes in to the practice complaining of reduced comfort with his lenses over the past week. He recently switched from the multipurpose solution you recommended to an own-brand solution.
Questions:
1. What slit lamp technique would you use to examine this patient for corneal staining?
A. Narrow beam
B. Low illumination
C. White light
D. Fluorescein and cobalt blue light
2. What is the best time of day to examine patients for solution-induced corneal staining?
A. Immediately after lens insertion
B. 2-4 hours after insertion
C. 6-8 hours after insertion
D. At the end of the daily wearing time
3. Slit lamp examination shows this patient has approximately 30 diffuse punctate spots on the cornea. What grade would you give to this extent of staining?
A. Grade 1
B. Grade 2
C. Grade 3
D. Grade 4
4. Which of the following management options are you most likely to consider first?
A. Refer for medical treatment
B. Switch to daily disposable lenses
C. Remove lenses until resolved and then resume lens wear using your recommended solution
D. Ocular lubricants
Answers:
1. The correct answer is D. Instilling fluorescein and using cobalt blue and yellow barrier filters is the best method for viewing corneal staining.
2. The correct answer is B. Studies have shown that the optimum time to examine for solutioninduced staining is 2- 4 hours after insertion.
3. The correct answer is B. A total of 21-40 punctate diffuse spots with no coalescing patches indicates Grade 2 extent of corneal staining.
4. The correct answer is C. Advise the patient only to use the care product you recommend and note the brand on his contact lens specification.