What you need to know
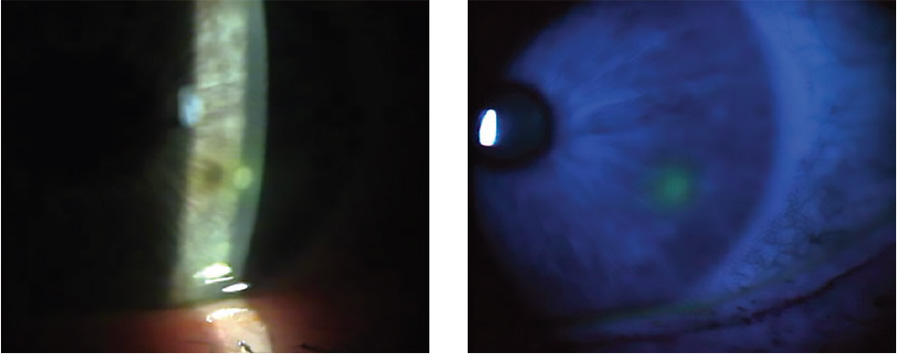
Slit Lamp Viewing:
• Direct illumination • Medium/high magnification (16-25x) • White light then with fluorescein, cobalt filter and yellow barrier filter • White light optical section to assess depth
Describing clinical appearance:
- Location: Superior, inferior, nasal, temporal; central or peripheral
- Size: Measure/estimate size, shape and depth and/or take a digital image
- Note presence or absence of corneal staining overlaying stromal opacity
Incidence:
- Rigid corneal lens (RCL) DW 0.01-004%
- Hydrogel DW 0.02-0.05%
- SiHy DW 0.12%
- Hydrogel overnight wear 0.09-0.20%
- SiHy overnight wear 0.18-0.25%
- Ortho-K all ages 0.08%
- Ortho-K children 0.14%
Aetiology:
Infection of compromised cornea (epithelial break, hypoxia) from invasion of bacteria (esp. pseudomonas spp. - principally aeruginosa), virus, fungus or amoebae with excavation of corneal epithelium, Bowman’s layer and stroma with infiltration and necrosis of tissue.
Risk factors:
Overnight wear, hypoxia, poor compliance and hygiene, swimming/showering in lenses, tap water, not storing CL case dry, male, smoking, trauma, poor general and ocular health (diabetes, respiratory disease), warm climates, socio-economic class, longer wearing periods, delay seeking treatment, high ametropia (>5D), younger age (15-25 years), lens case contamination, environmental influences.
Symptoms:
- Severe pain with rapid onset, photophobia, epiphora, severe redness, reduced vision (depends on location), discharge, lid swelling
- No improvement after lens removal, pain usually increases
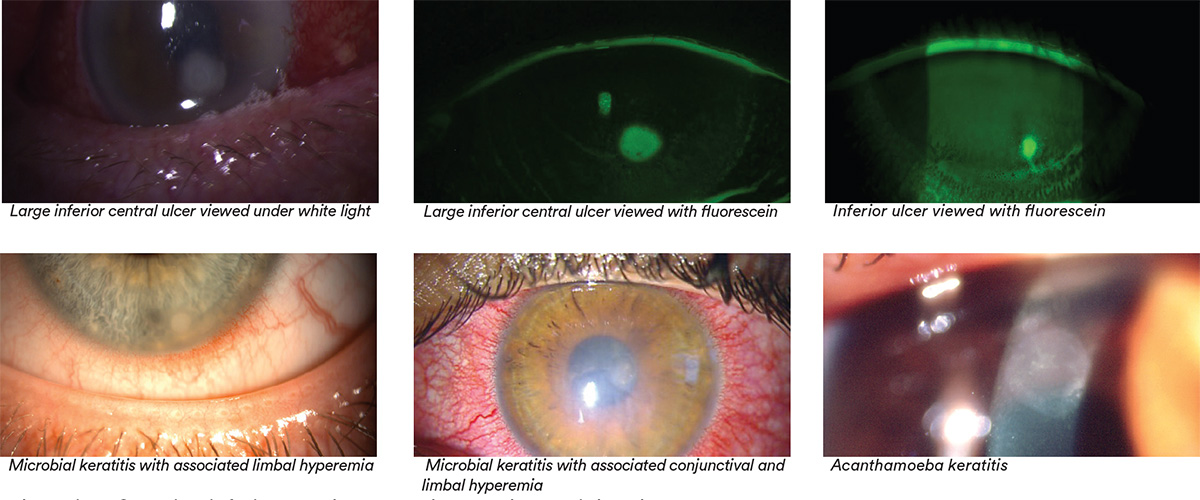
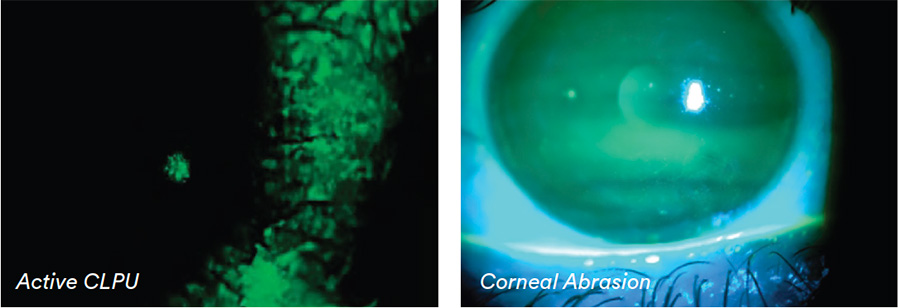
Signs:
- Examination can be difficult due to photophobia
- Full thickness epithelial defect with underlying infiltrate, Bowman’s layer and stroma affected
- Generally central, large (>1mm), unilateral, irregular appearance
- Severe hyperemia
- Anterior chamber activity (flare, hypopyon)
- Discharge and lid oedema
What you need to recommend to your patients
Management:
- Immediate discontinuation of lens wear — lenses and case not to be reused. (Retain both in case required for analysis.)
- Ocular emergency — urgent management required (via Optometry or Ophthalmology depending on local scope of practice), corneal scrape, close monitoring and medical treatment
- No patching
- Intensive treatment (cycloplegic, analgesic, antimicrobial, NSAIDs)
- Advise about risk factors — improve hygiene, care regimen and avoid tap water
- Refit with higher oxygen performance lens (SiHy, rigid corneal lens (RCL)), change to DW, refit into DD
- Reduce bioburden and micro-organism contamination
- Review case hygiene (inc. rubbing & tissue wiping) and replacement
Prognosis:
- Variable, depends on causative organism and position of lesion — often resolves with scar and vascularisation
- Improved with rapid intervention
- 14% lose 2 lines or more best corrected VA
- Better visual outcome with SiHy
Differential Diagnosis:
CLPU, dense corneal staining, corneal abrasion.
Further reading
- Arshad M et al. Water Exposure and the Risk of Contact Lens-Related Disease. Cornea 2019; 38: 791-797
- Bullimore M et al. The Risk of Microbial Keratitis With Overnight Corneal Reshaping Lenses; Optom Vis Sci 2013; 90(9): 937-944
- Carnt N et al. The diagnosis and management of contact lens-related microbial keratitis. Clin Exp Optom 2017; 100: 482-493
- Cheng KH et al. Incidence of contact lens associated microbial keratitis and its related morbidity. Lancet 1999; 354(9174): 181-185
- Dart J et al. Risk factors for microbial keratitis with contemporary contact lenses: a case-control study. Ophthalmology 2008; 115(10): 1647- 1654
- Fleiszig SMJ, Kroken A et al. Contact lens-related corneal infection: Intrinsic resistance and its compromise. Prog Retin Eye Res 2020; 76: 100804
- Green M et al. Trends in contact lens microbial keratitis 1999 to 2015: a retrospective clinical review. Clin Exp Ophthalmol 2019; 47: 726-732
- Keay L et al. Signs, symptoms, and comorbidities in contact lens-related microbial keratitis. Optom Vis Sci 2009; 86(7): 803-809
- Lam D et al. Incidence and risk factors for microbial keratitis in Hong Kong: comparison with Europe and North America. Eye 2002; 16(5): 608-618
- Morgan P et al. Incidence of keratitis of varying severity among contact lens wearers. Br J Ophthalmol 2005; 89: 430-436
- Nilsson S, Montan R. The hospitalised cases of contact lens induced keratitis in Sweden and their relationship to lens type and wear schedule. CLAO J 1994; 20 (2): 97-101
- Poggio E et al. The incidence of ulcerative keratitis among users of daily wear and extended wear soft contact lenses. New England J Med 1989; 321(12): 779-783
- Schein O et al. The incidence of microbial keratitis among wearers of a 30-day silicone hydrogel extended-wear contact lens. Ophthalmology 2005; 112(12):2172-2179 • Stapleton F et al. Risk factors with CL related suppurative keratitis. CLAO J 1993; 19(4): 204-210
- Stapleton F et al. The Incidence of Contact Lens–Related Microbial Keratitis in Australia. Ophthalmology 2008; 115(10): 1655–1662
- Wu YT et al. Contact lens hygiene compliance and lens case contamination: A review. Cont Lens Anterior Eye 2015; 38: 307-16
- Click here to review our Slit Lamp Techniques Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answers at the foot of the page to see whether it’s correct. Good luck!
History:
Patient JC is a 20-year-old male student who has worn monthly replacement hydrogel lenses for the past three years.
He attends for an emergency appointment late afternoon wearing his lenses and complaining of a very painful, watery red eye since this morning. He is suffering from intense photophobia making examination difficult.
JC reports he has been wearing his lenses regularly overnight.
Questions:
1. What slit-lamp techniques might you use to examine this patient’s cornea?
A. Fluorescein and cobalt blue filter
B. Direct illumination and medium/high magnification
C. Optical section
D. All of these
2. Which of the following features of suspected microbial keratitis would you record?
A. Shape and size of ulcer
B. Location
C. Underlying stromal opacity
D. All of these
3. What is the most likely risk factor associated with MK in this patient?
A. Poor lens fit
B. Overnight wear
C. Delay seeking treatment
D. Trauma
4. Which of the following management options would you be most likely to choose?
A. Advise to leave lenses out for a week then resume
B. Refit with silicone hydrogel lens and continue wear
C. Refer urgently for ophthalmological investigation
D. Patch the eye and see again in two days’ time
Answers:
1. Correct answer is D. All of these techniques have a role in assessing microbial keratitis and in differential diagnosis
2. Correct answer is D. All of these features, ideally supported by ocular photography, should be recorded
3. Correct answer is B. Overnight wear is the most obvious risk factor involved although the aetiology may be multi-factorial
4. Correct answer is C. Refer urgently as an ocular emergency for corneal scrape, close monitoring and medical treatment