What you need to know
Slit Lamp Viewing:
• Direct focal illumination • High magnification (25 - 40x) • Low light intensity
Describing Clinical Appearance:
Assessment of Tear Film:
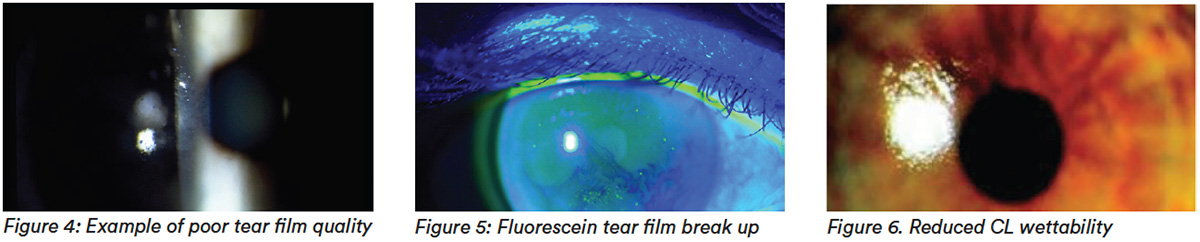
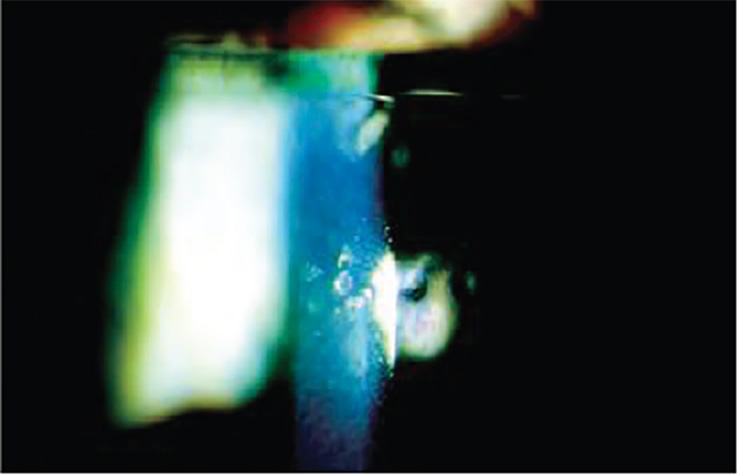
- General quality, such as frothing, foaming, particles – Slit Lamp
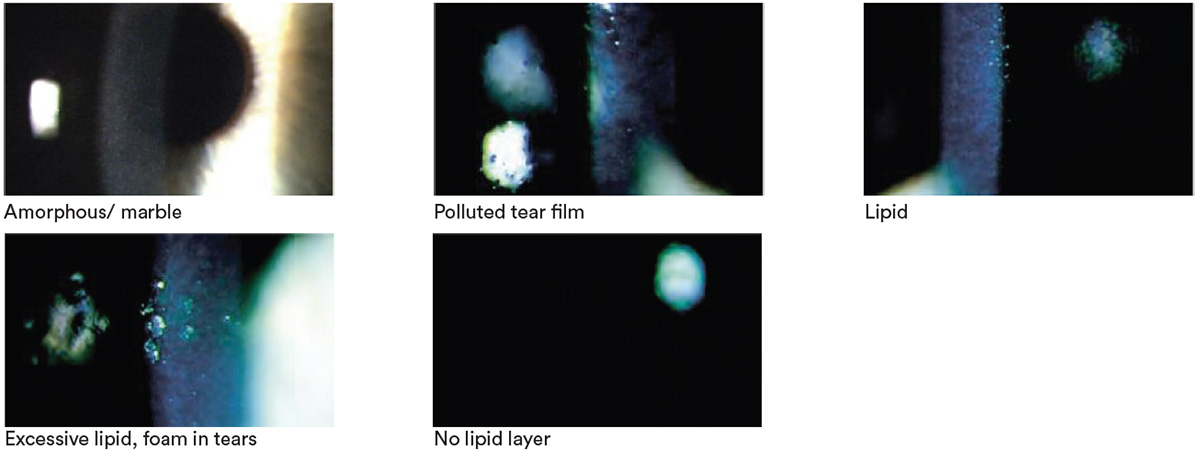
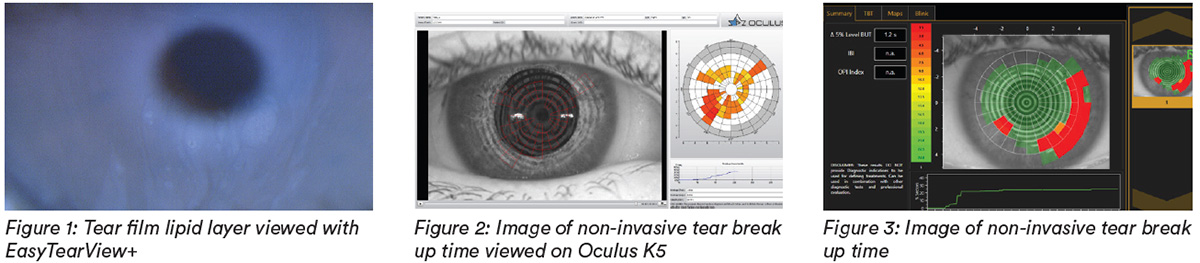
- Lipid layer presence – Interferometer (automated assessment or subjective grading) (top right)
- Tear stability through invasive (Fluorescein, FTBUT/ITBUT) and non-invasive tear film break-up time (NIBUT) – Keratometer, Topographer, Interferometer (automated or observer assessment)
- Tear osmolarity - Osmometer, to be conducted ahead of any invasive tests
Aetiology:
- Separation of tear film by CL into two layers (pre- and post-lens tear film) leads to thinner lipid layer, increased evaporation and destabilized tear film
- Poor meibum quality and expression
- Incomplete blinking, reduced blink rate affect tear exchange, spreading, drainage, meibum expression, ocular exposure
- Variation in individual tear chemistry (ocular physiology, medication, age, diet)
- CL material, design, wearing schedule, care regimen
- Cosmetics, soap contamination
- Environment (humidity, smoking, pollution)
Symptoms:
- Dryness symptoms including discomfort, grittiness and irritation - assess using questionnaire such as Ocular Surface Disease Index (OSDI), Contact Lens Dry Eye Questionnaires (CLDEQ-8)
- Blurred or variable vision
Signs:
- Low pre-ocular TBUT, poor tear mixing
- Thin or absent tear film lipid layer or excess lipid (debris in tear film),
- Reduced wettability, deposited CL
- Bulbar conjunctival hyperemia
- Superficial punctate corneal epithelial erosions
- Bulbar conjunctival staining
- Lid margin staining
- High tear osmolarity (>308 mOsmol/L) or interocular difference >8 mOsmol/L
What you need to recommend to your patients
Management:
- Manage all grades if signs or symptoms exist— improve tear film quality
- Treat any lid margin disease – lid hygiene, warm compresses, device-assisted thermal pulsation & expression in office, debridement
- Consider CL type (design, material, modality, replacement frequency and care system)
- Maintain good lens cleaning including rub and rinse step
- Use of lipid containing drops or sprays, visco-elastic agents or overnight lubricants
- Alter diet, Omega-3 oral supplements, alter environment, change cosmetics, blink training
- Consider Ortho-K – circumnavigates the need for CL wear in the open eye and its associated symptoms
Prognosis:
Good, unless fundamental imbalance of tear film (keratoconjunctivitis sicca)
Further reading
- Chalmers R et al. Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8) and opinion of contact lens performance. Optom Vis Sci 2012; 89(10): 1435-1442
- Craig J et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Contact Lens Interactions with the Tear Film Subcommittee. Invest Ophthalmol Vis Sci 2013 Oct; 54(11): TFOS123-56
- Downie L, Craig J. Tear film evaluation and management in soft contact lens wear: a systematic approach. Clin Exp Optom 2017 Sep; 100(5): 438-458
- Papas E et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Management and Therapy Subcommittee. Invest Ophthalmol Vis Sci 2013 Oct; 54 (11): TFOS183-203
- Tomlinson A et al. Tear film osmolarity: determination of a referent for dry eye diagnosis. Invest Ophthalmol Vis Sci 2006; 47(10): 4309-4315
- Wang M et al. Impact of blinking on ocular surface and tear film parameters. Ocul Surf 2018 Oct; 16 (4): 424-429
- Click here to review our Slit Lamp Techniques Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answer at the foot of the page to see whether it’s correct. Good luck!
History:
Patient TR is a 22-year-old clerical assistant who has worn daily disposable hydrogel contact lenses since the age of 16. She wears her lenses at least 16 hours a day and sometimes longer for nights out after work. She complains of dry, gritty eyes and problems seeing her computer screen towards the end of the working day
Questions:
1. What slit lamp technique would you use to examine this patient’s tear film?
A. Indirect retro illumination
B. Direct illumination, high magnification
C. Indirect illumination
D. Specular reflection
2. Slit lamp examination reveals debris in the tear film and hydrophobic spots on the lenses just after blinking but no tear foaming or lipid deposits. How would you describe her tear film quality?
A. Polluted tear film
B. Lipid
C. Excessive lipid
D. No lipid layer
3. Which of these investigative techniques is most likely to be useful?
A. Over-refraction
B. Measuring pre-ocular tear break-up time
C. Checking lens fit
D. Checking K readings
4. Which of the following management options would you be most likely to consider?
A. Switch to reusable lenses
B. Refit with RGP lenses
C. Discontinue lens wear
D. Advice on cosmetics, lid hygiene, warm compresses and blinking
Answers:
1. The correct answer is B. 25-40x magnification and direct illumination with low light intensity is best for examining tear film quality
2. The correct answer is A. Polluted tear film. Description of tear film quality depends on a number of observations. Use the suggested framework to make these as consistent as possible.
3. The correct answer is B. Removing the lenses, instilling fluorescein (below) and measuring tear break-up time is most likely to provide you with useful information

4. The correct answer is D. Manage all grades if symptoms occur and any or all of the advice listed in option D are the most likely for you to consider

