What you need to know
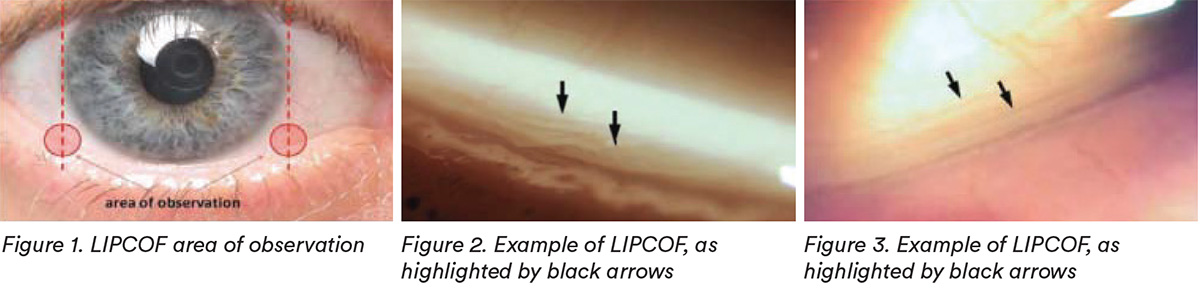
Slit Lamp Viewing:
• Diffuse beam • Medium magnification (18 - 27x) • Direct white illumination with no CL and in primary gaze • No use of vital dyes (fluorescein, lissamine green or rose bengal) • Evaluate in area perpendicular to temporal and nasal limbus (temporal LIPCOF and nasal LIPCOF) on bulbar conjunctiva above lower lid.
Grading:
A combined score (LIPCOF Sum) can be calculated by adding nasal and temporal LIPCOF grades
Grade 0: No conjunctival folds
Grade 1: One permanent and clear parallel fold
Grade 2: Two permanent and clear parallel folds (normally <0.2mm)
Grade 3: More than two permanent and clear parallel folds (normally >0.2mm)
Incidence:
- In non-CL wearers, 57% LIPCOF Sum of 1 or less (nasal LIPCOF grade plus temporal LIPCOF grade)
- Higher in symptomatic compared to non-symptomatic CL wearers
- In CL wear correlates with CL discomfort, lid wiper epitheliopathy, older age and lower mucin production
Aetiology:
- Possible causes are conjunctival looseness, decrease of elastic fibres, ageing or mechanical forces between lower lid and conjunctiva
Symptoms:
- Dryness
- Combine with non-invasive break-up time (NIBUT) and Ocular Surface Disease Index (OSDI) questionnaire as predictive assessment for dry eye symptoms in CL wearers
Signs:
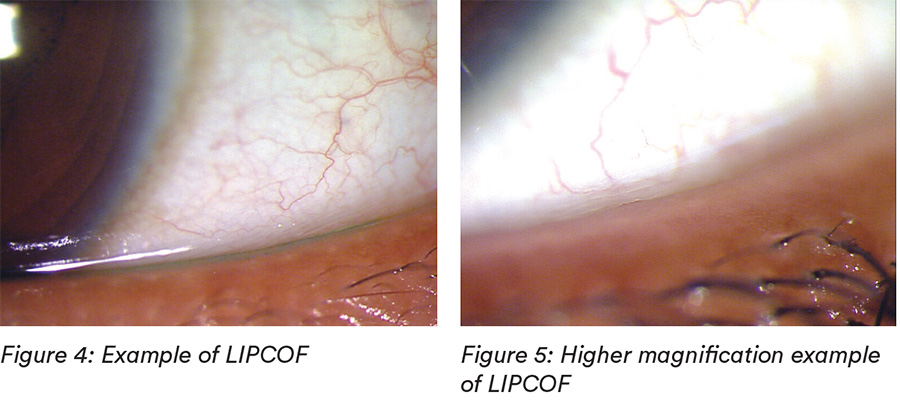
- Folds in temporal and nasal lower quadrants of bulbar conjunctiva, parallel to lower lid
What you need to recommend to your patients
Management:
- Manage ≥ grade 2 or if symptoms
- Refit with more lubricious lens surface
- Change lens type (SiHy to hydrogel) or wearing schedule (increase replacement frequency, reduce wearing time)
- Maintain good lens cleaning including rub and rinse step
- Manage any tear quality issues
- Rewetting drops or liposomal sprays
Prognosis:
Generally good resolution of symptoms with appropriate management.
Differential Diagnosis:

- Parallel permanent conjunctival folds, disrupted microfolds or conjunctival flaps (left)
- LIPCOF disappears when lower lid is lifted
Further reading
- Bandlitz S et al. Lid-parallel conjunctival fold (LIPCOF) morphology imaged by optical coherence tomography and its relationship to LIPCOF grade. Cont Lens Ant Eye 2019; 42(3): 299-303
- Berry M et al. Mucins and ocular signs in symptomatic and asymptomatic contact lens wear. Optom Vis Sci 2008; 85(10): E930-938
- Michel M et al. The effectiveness of questionnaires in the determination of contact lens induced dry eye. Ophthalmic Physiol Opt 2009; 29(5): 479-86
- Pult H et al. A novel method to predict the dry eye symptoms in new contact lens wearers. Optom Vis Sci 2009; 86(9): E1042-1050
- Pult H, Bandlitz S. Lid-Parallel Conjunctival Folds and Their Ability to Predict Dry Eye. Eye Contact Lens 2018; 44 Suppl 2: S113-S119.
- Pult H, & Riede-Pult B. Impact of soft contact lenses on lid-parallel conjunctival folds. Cont Lens Ant Eye 2019; 42(4): 415-419
- Tapaszto B et al: OCT Imaging of lid-parallel conjunctival folds in soft contact lens wearers. Optom Vis Sci 2011; 88: 1206-13.
- Click here to review our Slit Lamp Techniques Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answers at the foot of the page to see whether it’s correct. Good luck!
History:
Patient AC is a 56-year-old company director who has worn a variety of soft contact lenses over a period of nearly 35 years and is currently wearing monthly replacement silicone hydrogel lenses. She returns to the practice two months after her last check-up complaining of dry eyes

Questions:
1. What slit lamp technique would you use to examine this patient’s lids for LIPCOF?
A. Fluorescein dye and cobalt blue filter
B. Indirect illumination
C. Diffuse beam, medium magnification
D. Specular reflection
2. Two temporal conjunctival folds are visible. What grade would you give to the LIPCOF?
A. Grade 0
B. Grade 1
C. Grade 2
D. Grade 3
3. Which of the following dry eye assessments might you use for this patient?
A. Measure non-invasive break-up time (NIBUT)
B. Measure tear meniscus height to assess tear volume
C. Have the patient complete the OSDI questionnaire
D. Any of these options
4. Which of the following management options could you consider?
A. Refit with lenses with a more lubricious lens surface
B. Make sure the patient includes a rub and rinse step in the cleaning regime
C. Recommend rewetting drops or liposomal sprays
D. Any of these options
Answers:
1. The correct answer is C. A diffuse beam, 18-27x magnification and direct illumination is best for examining the conjunctiva for LIPCOF
2. The correct answer is C. Two permanent and clear parallel folds indicate grade 2 LIPCOF
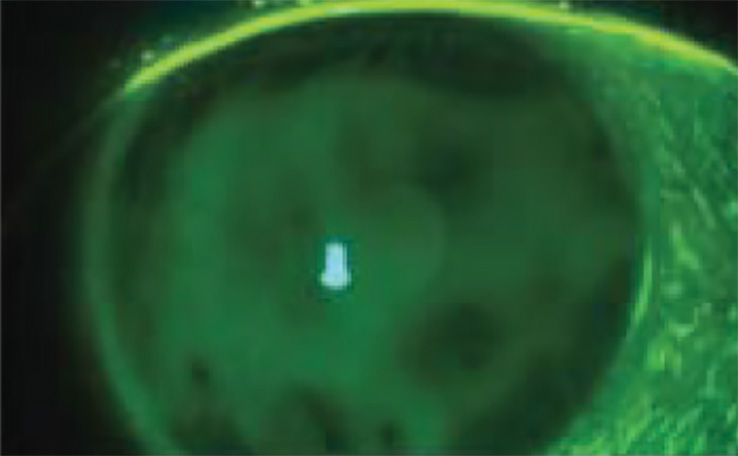
3. The correct answer is D. Tear film stability (below), tear volume and dry eye all correlate with LIPCOF so all these would be appropriate
4. The correct answer is D. LIPCOF grade 2 and over should be managed and any of these management options could be considered

