By Andy Cole and Clair Bulpin
Why initiate a contact lens conversation?

What do your practice staff and environment communicate?
Communication is so much more than words
Effective patient communication can:
- Improve clinical outcomes
- Make more efficient use of our time
- Increase patient value and build loyalty
To communicate well, use every patient interaction as an opportunity to really build rapport with your patients. Remember the old cliché that any conversation is a two-way process; being understood is a combination of what you say and do, and how others respond.
It’s more than the 30 minute consultation!
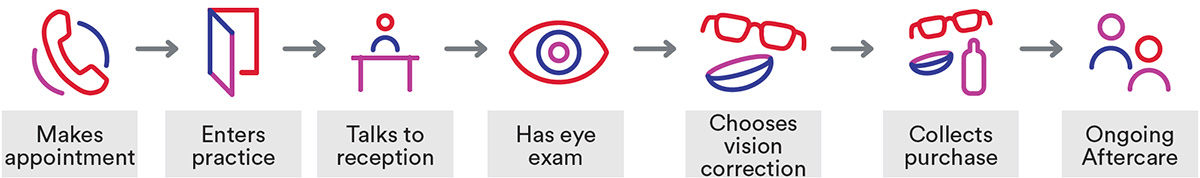
Patients see their eye care experience starting from the moment they book their appointment and only ending when they collect their purchase (see below).
Recognise the key points of contact
Skilled communicators understand the importance of key points of contact within the customer journey and how the handover between each member of the team is crucial.
Why take a patient-centred approach?
Dr Fiona Fylan (health psychologist) explains the importance of a partnership between the patient and eye care practitioner to agree the best outcome and how to achieve it.1
- The practitioner contributes their clinical knowledge
- The patient is the expert on their individual needs and requirements.
The GOC standards of practice detail how eye care practitioners should ‘Listen to patients and ensure they are at the heart of the decisions made about their care’.2
The patient-centred approach ensures that each conversation is tailored and specific to that individual, with relevant advice and recommendations forming a discussion rather than instruction.
What to look and listen for
While we may all like to consider ourselves as proficient communicators, our patients may well disagree.
Look out for barriers
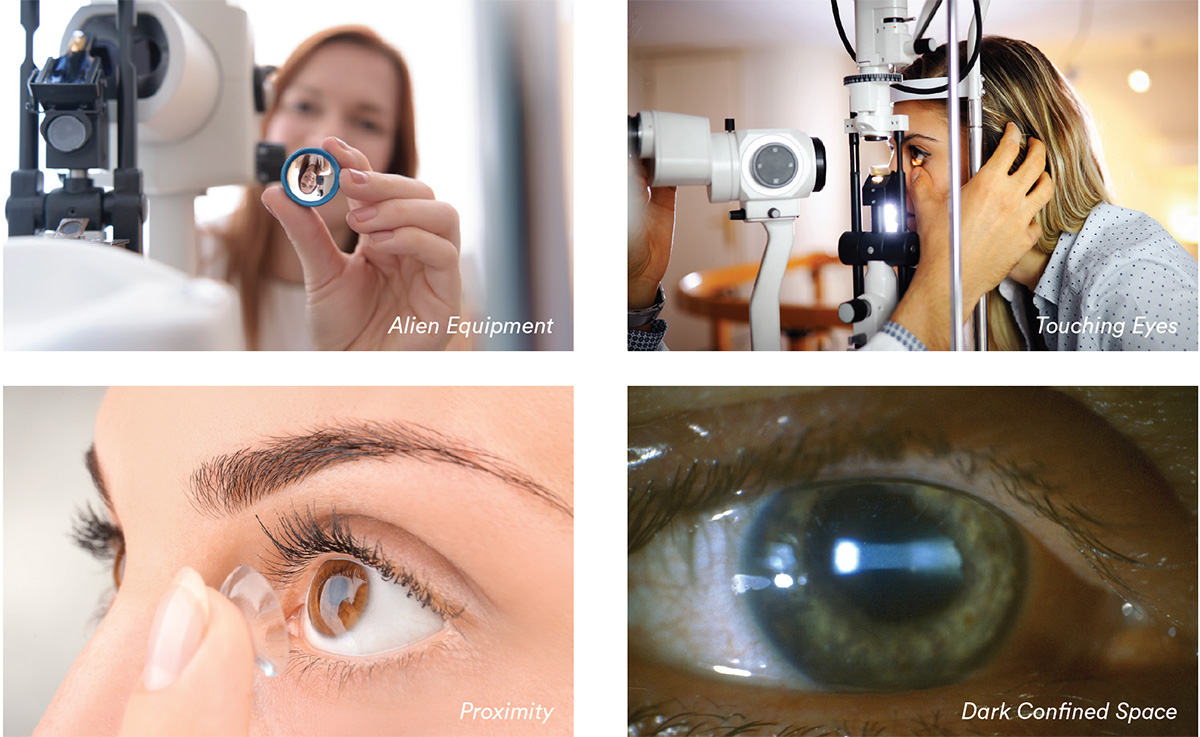
With new contact lens wearers, lack of information about what’s involved and apprehension about touching or putting something ‘in’ the eye means that there are greater barriers to overcome.
Listen
There is a difference between listening and hearing. Focusing on the information shared and concentrating on all elements of the communication is considered as active listening. This is often described as listening with all senses, so includes acknowledging body language and tone of voice alongside simply hearing the words. With active listening you demonstrate empathy which will help you achieve rapport.
There can be emotional, social or psychological reasons for trying contact lenses. You may discuss personal issues, such as how they feel about their appearance or how they’re viewed by others. Their interest in contact lenses may be sparked by defining moments in their lives, such as changing schools or getting married, that they might not otherwise discuss during the course of an eye examination.
When your patient shares these thoughts with you, and discusses how they feel, you know that you have achieved a good rapport.
What to say and do
Treat your patients how they want to be treated instead of how you want to be treated.
Build rapport with your patients
Rapport is the process by which two people become mutually responsive to each other and is the key to every successful interaction.
- Psychologist Will Schutz describes how the need to feel significant, competent and likeable are the three factors that underline rapport3
- Instead of fitting the patient in to your ‘routine’, think about establishing a relationship with each individual in a similar way that you would in social situations
- Building rapport with your patients will give you better information which, in turn, helps you make better decisions and higher quality recommendations
- By considering how you can establish and maintain rapport with your patient you will make much more efficient use of your consultation time
 Try to lose your comfort blanket
Try to lose your comfort blanket
Most practitioners begin appointments with the same well-oiled phrase. Using stock words and phrases, while often well meaning, lacks the sincerity of a genuine conversation.
 Treat everyone as an individual
Treat everyone as an individual
A ‘routine’ appointment can often seem to be just that to an eye care practitioner. However, it is anything but ‘routine’ to our patients. Ensure that every patient has your full attention and that their own individual specific needs and concerns are addressed.
![]()

 Identify your strengths and weaknesses
Identify your strengths and weaknesses
Identifying interactions which went well and felt good, alongside those that didn’t, can help you understand where your development needs lie. Asking colleagues for feedback can provide valuable insight and often highlights things you may not have considered yourself.
 Gain ‘concordance’ rather than compliance
Gain ‘concordance’ rather than compliance
It is much better for a patient to understand the ethos behind instructions, and gaining agreement on a process will drive great behaviours. Compliance is simply the act of following the rules, concordance strives for a deeper understanding and agreement between patient and eye care practitioner. To achieve concordance, you will need to ask more questions, using collaborative language, leading ultimately to greater success through a harmonious partnership.
 Make patients feel important
Make patients feel important
By being genuinely attentive and interested in your patient, you increase their feelings of importance within the interaction. Inviting them to feedback on a new lens or solution enhances their part in this interaction, and makes them more receptive to subsequent advice.