What you need to know
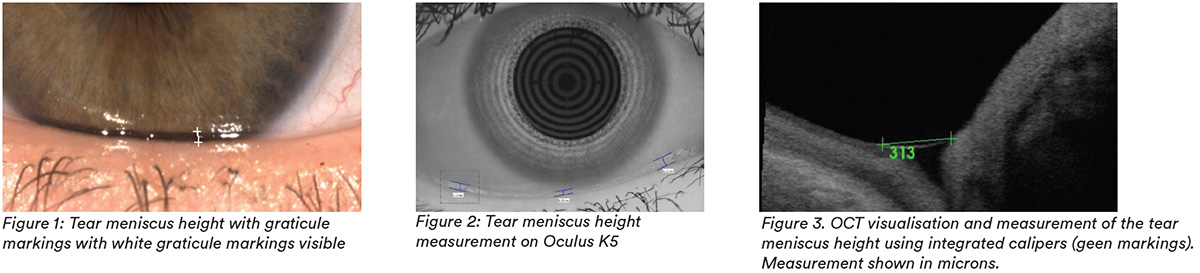
Slit Lamp Viewing:
• Direct focal illumination • High magnification (40x) • Rotate beam horizontally to align with the lower lid margin and adjust slit width until it appears to match the height of the tear prism, with patient in primary gaze with normal blinking
Describing Clinical Appearance:
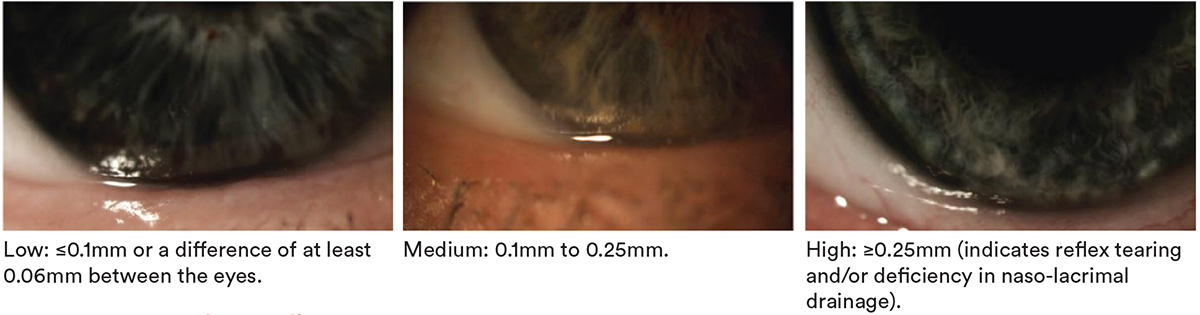
Tear meniscus height
Assessment of Tear Film:
- Tear volume on eye through non-invasive tear meniscus height – slit lamp with or without graticule, tear interference,optical coherence tomography.
- Tear production through invasive tests - Schirmer test, Phenol red thread test.
Aetiology:
- Multifactorial, including age, medication, systemic or ocular conditions, environment.
- Poor tear film exacerbated by presence of CL.
Symptoms:
- Dryness, discomfort, grittiness, irritation, sensitivity to adverse environments- assess using questionnaires such as Ocular Surface Disease Index (OSDI), Contact Lens Dry Eye Questionnaires (CLDEQ-8, CLDEQ-5)
- Blurred or variable vision
Signs:
- Reduced tear meniscus height, irregular tear meniscus (notching or scalloped edge) (top right image) concave tear profile
- Low Schirmer test scores (at 5 mins, normal >10mm, borderline 5-10mm, severe dry <5mm) or low Phenol red thread test scores (at 15 secs, dry eye <10mm)
What you need to recommend to your patients
Management:
- Address associated systemic or ocular conditions
- Manage any tear quality issues
- Assess prior to lens fit and during CL wear to manage appropriately
- Change lens type (design, material, modality, replacement frequency)
- Maintain good lens cleaning including rub and rinse step
- Change lens care solution
- Rewetting drop/ ocular lubricants
- Attention to nutrition or nutritional supplements (essential fatty acids)
- Environmental changes (humidifier)
- Tear retention measures (to reduce drainage and increase tear contact time) such as punctal plugs or surgery
- Consider Ortho-K – circumnavigates the need for CL wear in the open eye and its associated symptoms
Prognosis:
Generally good resolution of symptoms with appropeiate management unless intractable underlying systemic or ocular condition
Further reading
- Bitton E et al. Influence of the blink interval on tear meniscus height in soft contact lens and nonlens wearers. Eye Contact Lens 2010; 36:156-63.
- Chalmers R et al. Validation of the 5-Item Dry Eye Questionnaire (DEQ-5): Discrimination across self-assessed severity and aqueous tear deficient dry eye diagnoses. Cont Lens Ant Eye 2010; Apr 33(2): 55-60
- Chalmers R et al. Contact Lens Dry Eye Questionnaire-8 (CLDEQ-8) and opinion of contact lens performance. Optom Vis Sci 2012; 89(10): 1435-1442
- Craig J et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Contact Lens Interactions with the Tear Film Subcommittee. Invest Ophthalmol Vis Sci 2013 Oct; 54(11): TFOS123-156
- Downie L, Craig J. Tear film evaluation and management in soft contact lens wear: a systematic approach. Clin Exp Optom 2017 Sep; 100(5): 438-458
- Guillon J-P. Current clinical techniques to study the tear film and tear secretions. In The Tear Film: Structure, Function and Clinical Examination. Butterworth-Heinemann, Oxford, 2002
- Kokke K et al. Oral omega-6 essential fatty acid treatment in contact lens associated dry eye. Cont Lens Ant Eye 2008; Jun 31(3): 141-146; quiz 170
- Nagahara Y et al. Prominent Decrease of Tear Meniscus Height With Contact Lens Wear and Efficacy of Eye Drop Instillation. Eye Contact Lens 2015; 41: 318-22.
- Papas E et al. The TFOS International Workshop on Contact Lens Discomfort: Report of the Management and Therapy Subcommittee. Invest Ophthalmol Vis Sci 2013 Oct; 54(11): TFOS183-203
- Srinivasan S, et al. Apparent time-dependent differences in inferior tear meniscus height in human subjects with mild dry eye symptoms. Clin Exp Optom 2007; 90: 345-50.
- Click here to review our Slit Lamp Techniques Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answer at the foot of the page to see whether it’s correct. Good luck!
History:
Patient ME is a 55-year-old teacher who has worn monthly replacement hydrogel contact lenses for more than 30 years. Over the past few months she has needed to remove her lenses after 8 hours’ wear due to dry and irritated eyes, especially in heated and air-conditioned environments

Questions:
1. What methods would you use to examine this patient’s tear film quantity?
A. Phenol red thread test
B. Schirmer test
C. Measuring tear meniscus
D. Any of these methods
2. The tear film meniscus height is measured at 0.05mm using the eye-piece graticule. What grade would you record?
A. Low
B. Medium
C. High
3. What factors could be affecting this patient’s tear quantity?
A. Age
B. Environment
C. Medication
D. All these factors
4. Which of the following management options could you consider?
A. Discontinue lens wear
B. Modify lens fit
C. Refit with two-weekly replacement silicone hydrogel lenses that are known to perform well in challenging environments
D. Refit with RGP lenses
Answers:
1. The correct answer is D. These methods all assess tear quantity but measuring tear meniscus height is a non-invasive test and the recommended technique.
2. The correct answer is A. A tear meniscus height of less than 0.1mm is considered low and indicates reduced tear quantity.
3. The correct answer is D. Dry eye is multifactorial and any or all of these factors could be involved, as could systemic / other ocular conditions.
4. The correct answer is C. Changing to a silicone hydrogel lens material and replacing lenses more frequently are among the options to consider

