Cristina Schnider, OD, MBA, FAAO,
David Ruston, BSc FCOptom DipCL, FIACLE, FAAO
Introduction
In today’s world, presbyopia doesn’t have to be a major speed bump on the road of life. Today’s presbyopes, Generation X (Gen Xers), born between 1965 and 1980 (currently 40- 55) and Baby Boomers (born 1946-1964) enjoy more affluent and active lifestyles than ever before. Gen Xers are in their prime earning years, and Baby Boomers are just beginning to retire and enjoy life outside of work. Both groups are regular users of digital devices,1 which add to their visual demands, have significant disposable income,2 over two-thirds value looking younger3 and they are willing to spend money on products and procedures to maintain a youthful appearance ranging from hair colouring and teeth whitening to cosmetic surgery.4
Recently, an independent marketing research agency, IPSOS, with experience in healthcare including contact lenses, conducted a survey with 1000 representative consumers between the ages of 12 and 64 in both the United States (US) and United Kingdom (UK). In this survey5 they identified presbyopes as aged 40+ who either identified themselves as being presbyopic or who suffered from two or more symptoms of presbyopia. Using this definition, 386 UK contact lens wearers from 40-64 years of age in their Insight Global Incidence Tracker in December 2018, found that 93% of them said they expect to continue wearing contact lenses.5 The same agency surveyed 233 presbyopic contact lens wearers (same definition as above) and 584 non-presbyopic contact lens wearers and found that the presbyopic group were less likely to purchase contact lenses online than non-presbyopes, and more likely to purchase lenses where they received their eye exams.6
Yet despite the introduction of new multifocal contact lens designs by virtually every major manufacturer in recent years, the percentage of multifocal lenses fitted in practices globally remains low.7 As shown in Figure 1, the use of contact lenses drops sharply at the same time vision correction needs increase in the presbyopic population. Interestingly, as many as 4 in 10 contact lens wearers are 40+ years old yet according to a poll conducted by Gallup in 2015 only 9% of adults requiring an Add in that age group, received a recommendation for multifocal or monovision contact lenses as a means of correction.9 This is a massive untapped opportunity for contact lens practitioners not currently engaged in multifocal fitting to better meet the needs of their presbyopic patients.
.png)
Figure 1: The blue line represents all users of vision correction, and the red line contact lens wearers. The gap begins to widen between ages 35 and 44, the time when symptoms of presbyopia become evident. The shaded areas represent where opportunities to introduce multifocal contact lenses might be prioritised by eye care professionals.
Navigating a successful journey
A journey analogy is useful in thinking about exploring this opportunity – you have lots of different starting points (patients), destinations (goals), routes (options) to get them there (Figure 2). And while the presbyopia journey is generally but not always easy, it is usually worth it – 77% of people self reporting to wear multifocal contact lenses in a 2020 survey agreed that their contact lenses met their expectations10 and likely to tell their family and friends. So how do you get started? The first step in a successful journey is to make sure we are prepared and ready to go! 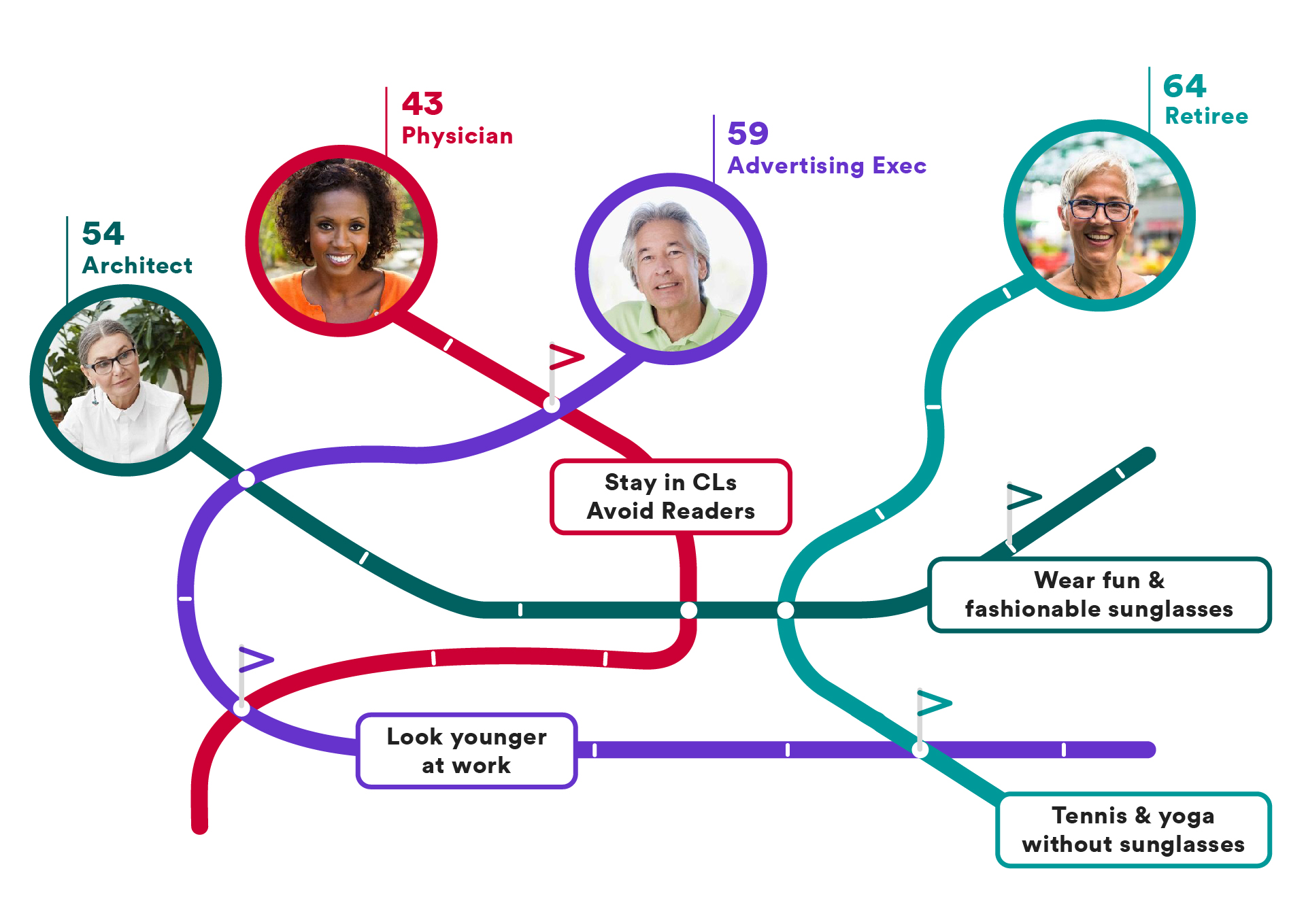
Figure 2: The presbyopic road map. A successful journey requires a destination – a mutual definition of success for contact lenses activities, selection of a vehicle (lens design, material and modality) and route (lenses plus spectacles to get them through presbyopia), as well as allowing for potential roadblocks or changing needs along the way. And of course, each patient will be unique, but there are many tools to help you get there.
Patient Considerations
An early presbyope who is already successfully wearing contact lenses is a great place to start. Studies11 say that nearly 4 in 10 contact lens wearers are 40+ years old and a large number wish to stay in lenses (responded ‘definitely/ probably would continue wearing contact lenses in the next 12 months’).8 These wearers can be prone to dry eye and lid conditions and should have a comprehensive evaluation of the ocular surface and lid status.

For any issues identified, addressing them prior to fitting multifocal contact lenses reduces the odds of dropping out significantly with each worsening grade of upper or lower eyelid meibomian gland (MG) plugging, upper eyelid meibum quality, and upper eyelid MG tortuosity.12 Simple interventions such as thermal pulsation13 or microblepharon exfoliation14 can have significant impact on tear film stability and evaporative dry eye.
Performing a new refraction is also essential, even with a seemingly well corrected patient. There is a documented progression toward more plus in distance refractions with age,15 and most multifocals perform best with a maximum plus distance refraction – adding +0.50 should easily blur the best corrected visual acuity line. It is also not advisable to rely on a current or previous contact lens prescription in lieu of a good spectacle refraction. Avoid patients with astigmatism exceeding 0.75DC. While there are new toric multifocals available, it is highly advisable to get very comfortable with spherical multifocals before attempting to add astigmatism to the mix.
Determine the lowest ‘‘functional’’ Add required to perform day to day activities. With a maximum plus distance sphere, we may expect a considerably lower Add than we require in their spectacle prescription. Avoid using visual acuity as a standard for determining the near addition.16-18 Instead, use a functional technique with relevant near target materials, font sizes and lighting, such as mobile phones, handheld devices or other simulations of near work that the patient will use routinely.
Use a variety of solutions
If you cook, you probably have different knives, pans, dishes and spices to help prepare the perfect meal. We wear different shoes for walking, running, playing tennis, special occasions. Every sport requires different equipment. It seems that presbyopic correction is one of the few areas of life where we expect one tool to do every job for our patients’ varied and busy lives! We have many vision correction tools available to us and we will have the most success if we employ them all – multifocal contact lenses, varifocals, top up reading glasses. It’s a matter of combining them to meet critical needs for appearance, convenience and functionality.

Identify the destination – what does success look like for that individual patient
Once you are prepared, it’s time to get going on the journey. Firstly, we need to identify the ‘destination’ – and more importantly, the contact lens-specific destination. Identify the situations where contact lenses are the ideal solution (and/or or glasses undesirable) and jointly agree on a measure of performance in the patient’s real world that they can use to judge success. This will be your ‘benchmark’ with the patient in determining success or whether any future tweaks are required. It’s helpful to also identify areas of flexibility, such activities where glasses would be acceptable.
These questions should highlight situations where contact lenses are the best option and will help identify a concrete definition of success for you and your patients.
A helpful question could be:
- If you could do ‘X’ without wearing glasses, would you consider these contact lenses successful?
Plan the best route – what are the specific needs we are trying to meet
Typically, there are multiple ways to get to your destination, and sometimes it’s just a matter of personal preference. On the presbyopia journey, it’s important to understand the preferences and pain points for your patient in planning how to get them to their destination. Never make assumptions for them; instead you need to ask. It’s also key to communicate to the patient that as their presbyopia evolves, so will the solutions that you will provide. Make sure you invest time to explore and understand their lifestyle and whether there are any specific situations/reasons for wanting an alternative to glasses. The three typical reasons are appearance, convenience and functionality, and each may lead to different solutions.
Appearance
People may choose to avoid reading glasses out of fear of ‘looking old’ in front of their friends or colleagues but have no absolute objection to wearing them in private. Others may actually enjoy wearing them in certain situations.
Helpful questions:
- Are there occasions when you wish that you weren’t seen wearing glasses?
- When are you happy to be seen wearing your glasses?
Convenience
If someone is on the move a lot between meetings, different projects in the home, or many activities with varying distance and near tasks, having to locate their readers may be very frustrating and varifocals may be awkward. Solutions could include having multiple pairs of readers staged around the house or workplace, standard and/or 'vocational' varifocals, but this is also a great opportunity to suggest multifocal contact lenses which may provide the convenience and practical solution they require.
Helpful questions:
- Which work or social occasions do you find wearing glasses really annoying or impractical?
- Which activities would you consider glasses to be more acceptable?
Functionality
Some multifocal glasses have been shown to impair depth perception and edge‐contrast sensitivity at critical distances for detecting obstacles in the environment, and this has been associated with trips and falls in the elderly.19,20 In fact, the effect was demonstrated for bifocals, trifocals and varifocals, so appears to be an effect of looking through plus powered additions generally. If a patient has concerns about varifocals while driving or navigating stairs for example, contact lenses could help in those situations, and varifocal glasses could still be used in more sedentary situations.
Helpful questions:
- Are there any situations where you are concerned when wearing your glasses such as driving or navigating the stairs?
- Are there any occasions when you feel your glasses are uncomfortable or causing you concern?
Multifocal Contact Lens Design Options
In recent years, consensus has become quite clear around the monovision versus multifocal question, and the science is overwhelming in favour of multifocal contact lenses.21 Monovision reduces binocularity, binocular summation and thereby contrast sensitivity and offers a limited window of success for patients – essentially wasting the period when adapting to multifocal contact lenses is arguably easiest.22,23 Further, several studies show that when exposed to both monovision and multifocal lenses, the preference is for multifocals for both early and more mature presbyopes,16,23-25 thus helping us keep them satisfactorily corrected through the evolution of their presbyopia.
With rare exceptions, today’s soft multifocal lenses are mostly either centre near aspheric designs, or a zonal aspheric system consisting of a centre near design paired with a centre distance design – an evolved version of modified monovision. Among the centre near designs, only one also offers pupil size optimisation to account for pupil size changes with age and refractive error, and a hybrid aspheric centre/ spherical periphery design for improved centration. These are important considerations as pupil size is known to vary with both refraction and age, with myopes and younger patients having larger pupils than hyperopes and older patients.26-28 The desired optical design will be compromised if any mismatch between the pupil size and the optical design occurs.29 Also, positioning the near optics in the centre of the pupil ensures that those powers will be available across a range of luminance for a patient with a given age and refractive error (Figure 3).
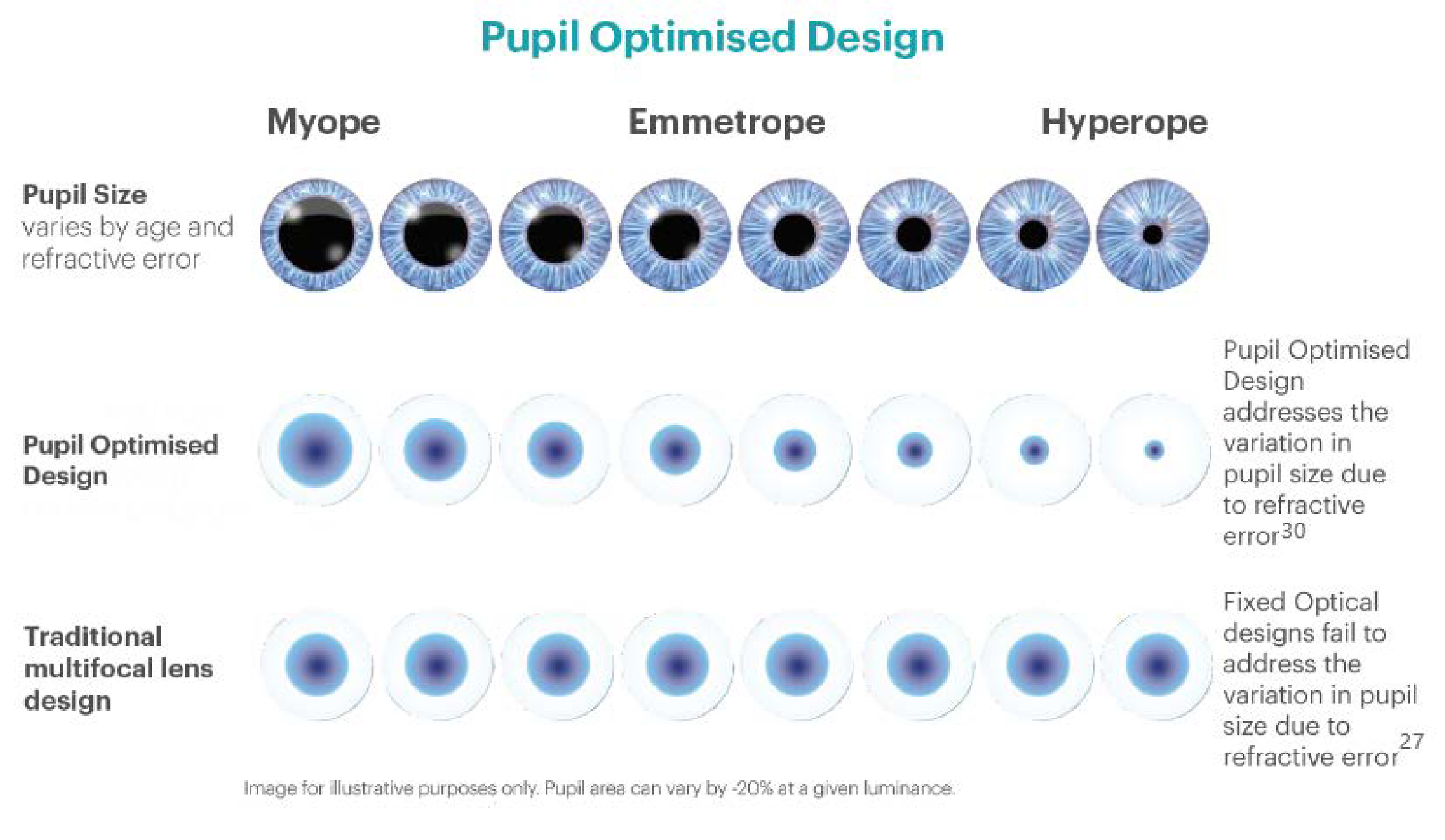
Note: For illustrative purposes only. Pupil area can vary ~20% at a given luminance.
Figure 3. Illustration of how pupil size varies across the refractive range and how optimisation of the multifocal design helps to place the range of powers from near to distance, within the pupil area.
The trick is to ensure that the intermediate and distance optics are also available and optimised within the given range of pupil sizes. It also follows, that centration of these complicated optics over generally smaller pupils is also critical as decentred multifocal contact lenses induce significant amounts of coma, a higher order aberration.31
These factors should all be considered when deciding which fitting banks should be available within the practice and when selecting a lens of first choice. It is certainly not necessary to carry all the possible designs but having two that offer unique fitting approaches is probably wise, with an overall preferred design to act as first choice. In addition, with the complexities inherent in multifocal contact lens fitting, having consistency in designs across materials and modalities within a manufacturer’s range has some advantages.
Lens Material, Modality and other features
Having access to both hydrogel and silicone hydrogel materials, as well as both daily disposable and reusable lenses in the practice enables you to meet a wider range of patient needs. Hydrogels are known for their demonstrated ability to maintain a low inflammatory response32 and they provide acceptable levels of corneal oxygenation with a low infection risk profile when worn for daily wear33 whereas silicone hydrogels provide improved corneal physiology from decreased hypoxia across a wide range of powers and thicknesses.33,34 Daily disposability offers great flexibility and convenience and reusable lenses offer a cost-effective option for many wearers depending on frequency of use.
The Detour – tweaks we can make to get the best outcome
As 2020 demonstrated, life doesn’t always go as planned, and sometimes we will need to make course adjustments. Keep in mind that with multifocal contact lenses, very small tweaks can make large differences. There are a few hints that will help you determine when to make a small adjustment, and when to make a radical course correction! Always follow the fitting guide for that brand of lens and avoid making changes until after the patient has experienced real-world vision with their multifocal lenses for several days. Always follow the fit guide, but general guidance is as follows:
- Always use real world near situations and materials to evaluate range and near functionality, instead of a reading chart.
- Limit lens changes to 1 or 2 maximum; if not successful, change lens design or try again on another occasion as motivations can change when people experience the ongoing challenges of presbyopia.
- Alter the environment (improve lighting, change text size or working distance) to enhance near performance.
- Use distance or reading glasses where vision is not sharp enough such as theatre, cinema and reading a menu in low lighting.

Why the journey is worth it
Fitting multifocal contact lenses provides a great opportunity to gain personal and professional satisfaction. Once you experience the ‘wow’ moment when a presbyopic patient realises they can actually do the things that matter to them without glasses, you’ll want to do it again and again. It’s a bit like fitting glasses or contact lenses to a young myope who didn’t realise what they were missing in the world – the reactions of successful patients are immensely satisfying! Dedicating yourself to a positive and flexible approach to fitting presbyopic patients with multifocal contact lenses provides a great opportunity to gain not only this satisfaction but to differentiate yourself and your practice.
The benefits of multifocal contact lens fitting to your practice can be summed up in ‘Three R’s’:
- Retention – The chances are that you have a wealth of potential patients already in your practice. By fitting the current contact lens wearers who are beginning to experience early signs of presbyopia, you have an excellent chance to help them continue to appreciate the benefits of contact lenses throughout presbyopia and retain them in your practice. Chair time will be reduced compared to a non-contact lens wearing patient and these patients can be highly motivated to stay in contact lenses. And if you occasionally need to add a form of spectacle vision correction to supplement in cases of unusual or more extreme need, don’t present it as a failure, but as just another tool in your tool box to help them on their journey. Just having the conversation about options and exploring options can create tremendous loyalty to your practice.
- Referrals – Never underestimate the power and pervasiveness of the ‘40- something grapevine’. Presbyopic patients have loads of presbyopic friends and being the only one not borrowing readers or using their phone torch to see the menu at a restaurant is sure to attract attention and generate questions. And presbyopes have families as well, so you may gain younger patients as an added benefit.
- Revenue – Confidently fitting multifocal lenses is still a relatively rare skill, and a specialty, so do charge appropriately for your services. It is well established that when looking at at all income to the practice, a contact lens patient is significantly more profitable over the long term than a spectacle-only patient.35 Successful multifocal contact lens patients will virtually always be dual wearers of contact lenses and glasses.
And finally, have fun, use all your available tools, always follow the manufacturer’s fit guide and be proactive about offering multifocal contact lenses to both current contact lens wearers as well as to new presbyopes. Persist even when patients choose not to try them as a seed planted this year could bear fruit in the future.



