What you need to know
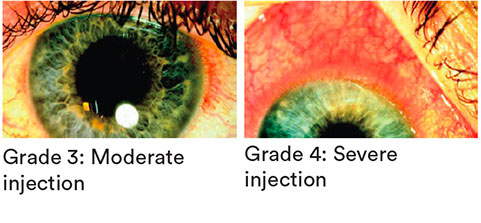
Slit Lamp Viewing:
• Diffuse beam • Medium magnification (16x) • Direct illumination
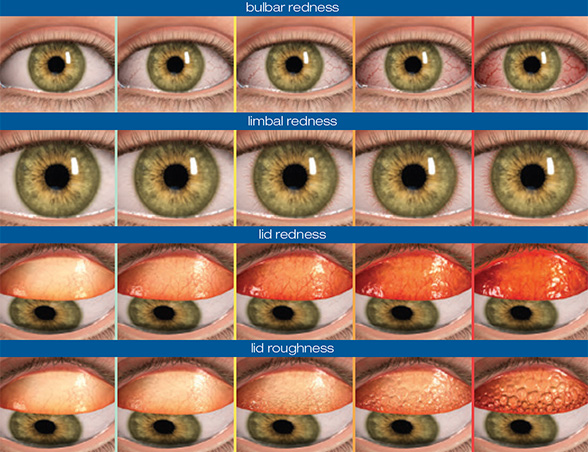
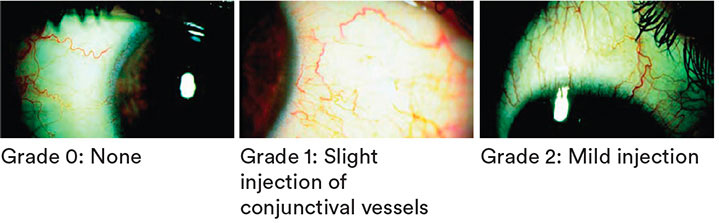
Grading:
Position: Superior, nasal, inferior, temporal
Incidence:
- 15-20% CL wearers, with 20-35% clinically significant
- Approximately 15% non-CL wearers ≥ grade 2
Aetiology:
- Solution sensitivity.
- Dry eye symptomatology or pathological dry eye - Keratoconjunctivitis Sicca (KCS).
- Allergic reaction.
- Infection — Microbial Keratitis (MK).
- Inflammation — Contact Lens Associated Red Eye (CLARE), Contact Lens Peripheral Ulcer (CLPU), Infiltrative Keratitis (IK) etc.
- Mechanical — poor lens fit, trauma.
- Metabolic — Corneal hypoxia, hypercapnia.
- Poor general health (especially influenza, throat infection or substance abuse).
- Scleral lenses – blood vessel compression, tightly fitting lens, lens adhesion.
Symptoms:
- May be asymptomatic — depends on cause
- Associated with CL intolerance, dryness, burning and itching
Signs:
- Bulbar conjunctival redness can be localised or diffuse
- Amount and pattern depend on lens type:
- rigid corneal lens wearers tend to exhibit this along the horizontal meridian (chronic drying)
- hydrogel lens wearers’ hyperemia tends to be diffuse
- scleral lens wearers’ hyperemia usually localised to area of lens compression / impingement – where circumferential, can indicate hypoxia / lactic acid accumulation in the post lens tear film
What you need to recommend to your patients
Management:
- Manage if ≥ grade 2 or if ≥ 1 grading scale increase or if symptoms occur
- Lens wear may continue if symptoms allow
- Remove the cause
- Switch to DD if aetiology is related to allergy
- Refit with higher oxygen performance materials (especially if hyperaemia is primarily located around the limbal region)
- Change lens material to reduce dryness
- Ocular lubricants
- Attend to any lid abnormalities (blepharitis; Demodex presence; MGD)
- Scleral lenses:
- Lens compression related - alter lens fit to reduce compression
- Toxicity related – increase lens material Dk/t and decrease central lens clearance where possible
Prognosis:
Good — although some wearers always exhibit some degree of bulbar hyperaemia
Differential Diagnosis:
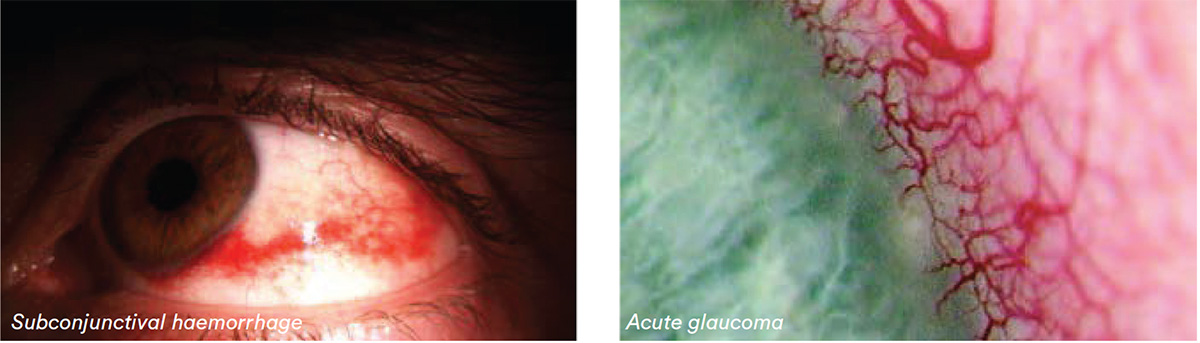
Subconjunctival haemorrhage, conjunctivitis, keratitis, uveitis, acute glaucoma
Further reading
- Efron N. Contact lens induced conjunctival hyperemia. Optician 1997; 213(5591): 22-27
- Huntjens B et al. Evaluating a new objective grading software for conjunctival hyperaemia. Cont Lens Anterior Eye 2020; 43: 137-143
- Guillon M, Shah D. Objective measurement of CL induced conjunctival redness. Optom Vis Sci 1996; 73(9): 595-605
- Murphy PJ et al. How red is a white eye? Clinical grading of normal conjunctival hyperaemia. Eye (Lond) 2007; 21: 633-8
- Pritchard N et al. Ocular and subjective responses to frequent replacement of daily wear soft contact lenses. CLAO J 1996; 22(1): 53-59
- Pult H et al. Limbal and bulbar hyperaemia in normal eyes. Ophthalmic Physiol Opt 2008; 28: 13-20
- Schulze M et al. The perceived bulbar redness of clinical grading scales. Optom Vis Sci 2009; 86: E1250-8
Click here to review our Slit Lamp Technique Videos
Patient case study
When you have read this guide and our recommended resources, why not take part in the Johnson & Johnson Institute self-assessment quiz to test your clinical diagnostic and management skills. Choose only one answer to each question then check the answers at the foot of the page to see whether it’s correct. Good luck!
History:
Patient GC is a 19-year-old university student who has worn daily disposable hydrogel lenses for sports and social use for the past three years. He wears his lenses 4-5 times a week for football training, matches and social events. At a routine aftercare appointment he presents with red, slightly sore eyes and reports that he has worn his lenses for the past 36 hours without removal.

Questions:
1. What slit lamp technique would you use to examine this patient’s bulbar conjunctiva?
A. High magnification, narrow beam
B. Indirect retro illumination
C. Direct illumination, medium magnification
D. Specular reflection
2. What grade would you give to his bulbar redness?
A. Grade 1
B. Grade 2
C. Grade 3
D. Grade 4
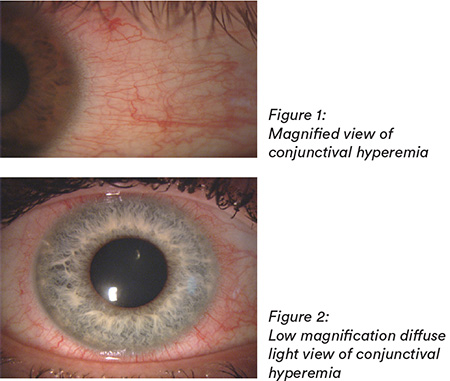
3. Which of the following techniques is most appropriate to the differential diagnosis of bulbar redness?
A. Slit lamp examination of the cornea
B. Keratometry
C. Over-refraction
D. Checking lens fit
4. Which of the following management options could you consider?
A. Emphasise the need to discard lenses daily and neverwear them overnight
B. Confirm spectacle Rx up to date
C. Re-emphasise the importance of hygiene
D. All of these options
Answers:
1. The correct answer is C. Using a diffuse beam, 16x magnification and direct illumination is best for examining the bulbar conjunctiva.
2. The correct answer is C. The patient’s bulbar conjunctiva shows moderate redness and should be graded 3.
3. The correct answer is A. Check carefully with high magnification for any corneal involvement such as infiltratitve keratitis (right).
4. The correct answer is D. If the cornea is not involved, continue lens wear, manage WT and hygiene and ensure spectacles current.